循环肿瘤细胞(CTC)逐步纳入乳腺癌肿瘤分期系统
2018-06-01 MedSci MedSci原创
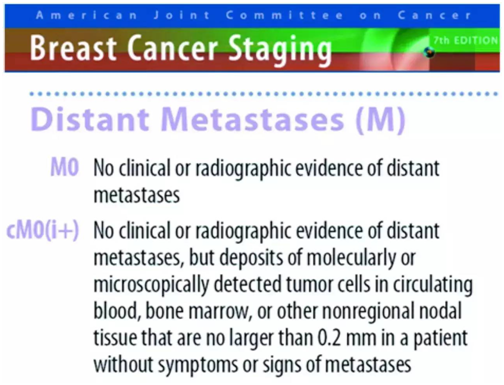
早在2010年美国癌症联合委员会AJCC制定的《肿瘤分期指南》(《Cancer Staging Manuel》)中,已把CTC列入TNM分期系统,作为一个新的M分期(远端转移)标准,列为cM0(i+)分期,出现在M0和M1之间。NCCN乳腺癌临床实践指南2017.V3 2017年底, NCCN指南(乳腺癌)2017.v3版也正式引入cM0(i+)分期,再次确认了引入CTC完
早在2010年美国癌症联合委员会AJCC制定的《肿瘤分期指南》(《Cancer Staging Manuel》)中,已把CTC列入TNM分期系统,作为一个新的M分期(远端转移)标准,列为cM0(i+)分期,出现在M0和M1之间。
2017年底, NCCN指南(乳腺癌)2017.v3版也正式引入cM0(i+)分期,再次确认了引入CTC完善肿瘤分期系统的重要意义。
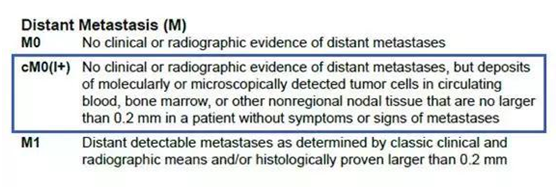
美国AJCC指南(第八版)
2018年1月1日在全球启用的AJCC第八版癌症分期系统中,除保留cM0(i+)分期外,更进一步明确了CTC检测的临床价值。最新指南将CTC列为继ER/PR、HER2、Ki67和肿瘤组织学分级四项生物学指标之后的又一项乳腺癌预后评估工具。
新版指南认为临床晚期乳腺癌外周血CTC≥5个/7.5ml,临床早期乳腺癌外周血CTC≥1个/7.5ml提示预后不良,证据水平为II级(AJCC Level of Evidence II)通过指南的逐步完善,循环肿瘤细胞(CTC)已正式进入肿瘤分期系统,完善肿瘤分期体系,为肿瘤的诊断与预后的评估提供更全面的指导。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#肿瘤分期#
47
#CTC#
37
#肿瘤细胞#
29
#循环肿瘤细胞#
52