JAMA:塞来昔布联合FOLFOX标准辅助化疗对结肠癌患者无病生存率的影响
2021-04-07 MedSci原创 MedSci原创
对于III期结肠癌患者中,在FOLFOX标准辅助化疗方案中加入塞来昔布对患者3年无病生存率无提高作用
尽管结直肠癌的预防和治疗已获得了显著进步,但2021年美国预计结直肠癌死亡人数将达到52980 人,全球结直肠癌死亡人数将超过915880 人。临床统计发现,80%结肠直肠癌患者最初并没有出现转移,但约50%的区域淋巴结阳性(III期)患者会在前5年内复发。在观察性和随机研究中,环氧合酶2(COX-2)抑制剂与降低结直肠息肉和肿瘤风险有关。

近日研究人员考察了在氟尿嘧啶、亚叶酸钙和奥沙利铂(FOLFOX)辅助化疗方案基础上,添加塞来昔布对III期结肠癌患者无病生存率的影响。

本次III期临床研究在美国及加拿大开展,2526名III期结肠癌患者参与,随访至2020年8月10日,参与者每2周进行1次FOLFOX化疗,持续3或6个月,在3年内,随机接受塞来昔布(每日口服400毫克;n=1263)或安慰剂(n=1261)治疗。研究的主要终点为无病生存率,次要终点包括总生存率、不良事件和心血管特异性事件。
参与者平均年龄61.0岁,1134名女性,2524名患者数据被纳入初步分析。治疗依从性方面,持续用药治疗2.75年以上或持续治疗直至疾病复发、死亡或不可接受的不良事件,塞来昔布组为70.8%,安慰剂组为69.9%。6年随访中,塞来昔布组共有337名患者出现疾病复发或死亡,而安慰剂组363名,塞来昔布组患者的3年无病生存率为76.3%,安慰剂组患者为73.4%(疾病复发或死亡的危险比[HR],0.89)。在指定辅助化疗持续时间内,塞来昔布治疗对无病生存率无显著影响。塞来昔布组5年总生存率为84.3%,安慰剂组为81.6%(死亡HR为0.86)。塞来昔布组14.6%的患者在接受FOLFOX治疗时出现高血压(任何级别),安慰剂组有10.9%.完成FOLFOX治疗后,塞来昔布组和安慰剂组肌酐水平升高2级或更高发生率分别为1.7%和0.5%。
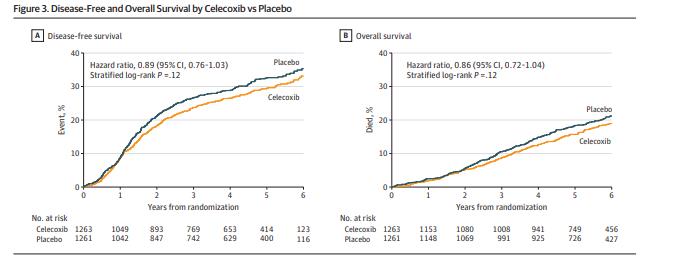
组间无病生存率及总生存率差异
对于III期结肠癌患者中,在FOLFOX标准辅助化疗方案中加入塞来昔布对患者3年无病生存率无提高作用。
原始出处
Jeffrey A. Meyerhardt et al. Effect of Celecoxib vs Placebo Added to Standard Adjuvant Therapy on Disease-Free Survival Among Patients With Stage III Colon Cancer The CALGB/SWOG 80702 (Alliance) Randomized Clinical Trial .JAMA. April 6, 2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#生存率#
74
#塞来昔布#
95
#FOLFOX#
85
明白了没有提高作用
0
无提高作用
131
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
93
学习了
134
学习了
121
学习了
90