“金标准”冠脉造影也会使诈,别TA被骗啦!
2018-04-28 人间世 医学界心血管频道
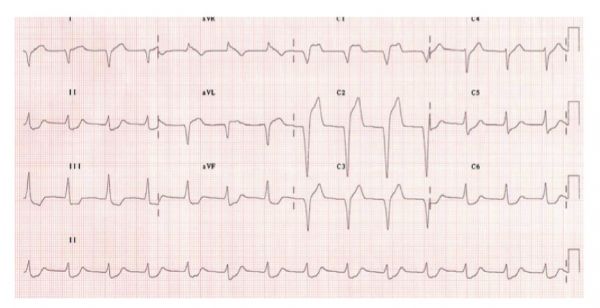
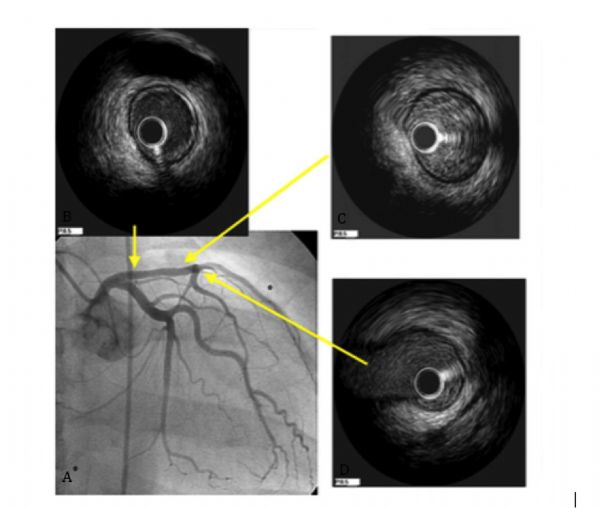
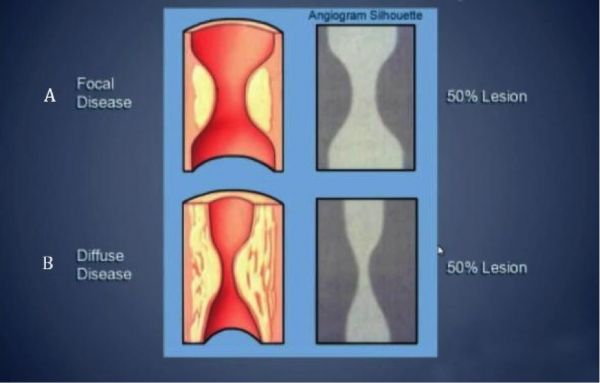
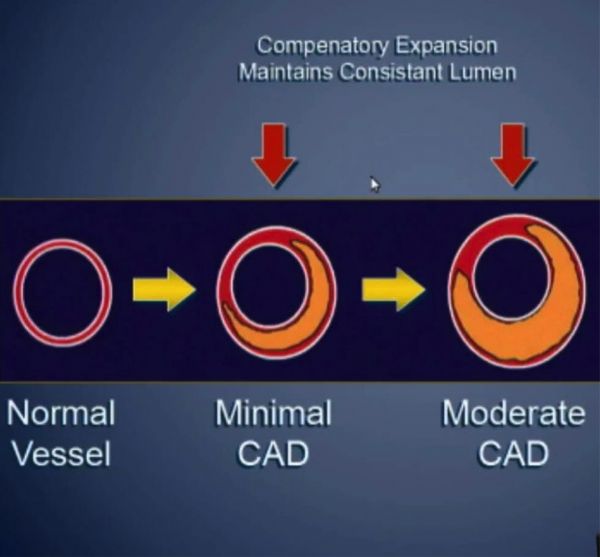
对于冠心病而言,冠脉造影一直是其诊断的“金标准”,它的“含金量”已经在长期临床工作中得到了很好的验证,但是“金无足赤”,冠脉造影也有自己的局限,今天我们就聊聊冠脉造影那不得不说的故事。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#金标准#
68
好
97
学习学习
107
#冠脉造影#
87
#造影#
69
厉害了我的哥
107
学习学习.继续关注
117
好好好好好好好好
93