FASEB J:电针疗法可以改善血糖的调节
2017-04-18 枫丹白露 medicalxpress
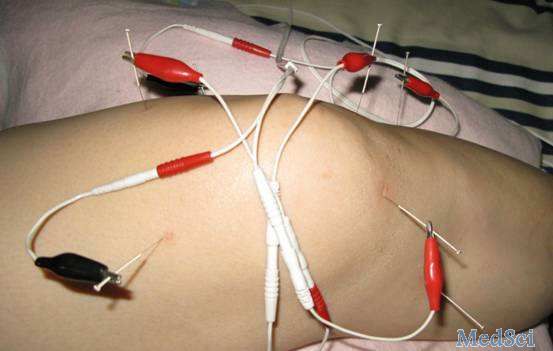
【电针疗法可能会改善超重和肥胖妇女血糖的调节】对于超重或肥胖且无法锻炼的妇女,《美国实验生物学学会联合会杂志》上发表的新研究表明,将针灸与电流结合起来可能有所帮助。在报告中,一个国际研究团队使用电针来刺激肌肉收缩,从而改善血糖调节。这项研究还可能有利于妇女中最常见的激素失调引起的多囊卵巢综合征(PCOS),其与糖尿病前期和发展为2型糖尿病的风险增加有关。瑞典斯德哥尔摩卡罗林斯卡研究所生理和药理学与
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#电针#
85
#FAS#
80
祖国医学博大精深
92
好好研究研究
118
阅读了谢谢分享
121
依然不错
97
感谢分享一下!
93
神奇
67