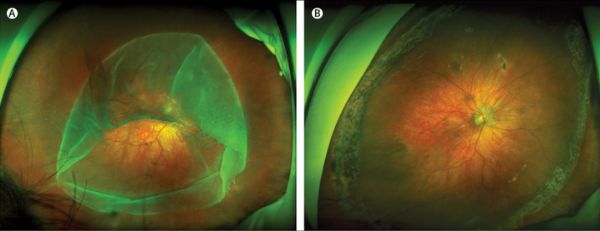
NAT COMMUN:利用CRISPR治疗视网膜色素变性
2017-04-05 佚名 生物通
CRISPR-Cas9基因组编辑技术给分子生物学领域带来了一场变革。研究者们只需使用细菌核酸酶Cas9和引导酶切位点的短RNA,就能够在活体生物中有效敲除或者改变基因序列,这为许多疾病的治疗带来了新希望。CRISPR-Cas9基因组编辑技术给分子生物学领域带来了一场变革。研究者们只需使用细菌核酸酶Cas9和引导酶切位点的短RNA,就能够在活体生物中有效敲除或者改变基因序列,这为许多疾病的治疗带
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#色素#
32
#Nat#
38
#视网膜色素变性#
40
#COMMUN#
36
#视网膜#
34
#CRISPR#
29
#变性#
33