BMJ:小剂量药物相比,小梁切除术具有相似的生活质量和安全性,且眼压更低。
2021-05-13 梅斯医学 MedSci原创
小剂量药物相比,小梁切除术具有相似的生活质量和安全性,并且眼压更低。
青光眼是一种慢性进行性眼病,对日常生活的许多方面都有实质性的不利影响。
开角型青光眼最初会影响周围的视力。晚期开角型青光眼患者会出现严重的视野缺失,侵占中心视力,最终降低视力。视野严重受限会降低生活质量,增加跌倒和骨折的风险。双眼都患有晚期开角型青光眼的人,即使视力良好,也可能有资格被认证为严重视力障碍。
有效的治疗可以控制疾病,防止视力进一步下降,从而防止失明。降低眼压是最有效的青光眼治疗方法。在诊断后的初始阶段更好地控制眼压可以减少进一步发展的风险。

Pixabay
近日,英国爱丁堡大学研究团队发表在BMJ上的研究显示,小剂量药物相比,小梁切除术具有相似的生活质量和安全性,并且眼压更低。

该研究在英国27个眼科中心进行,453位参与者在2014年6月3日至2017年5月31日期间至少一只眼睛出现了新诊断的晚期开角型青光眼(Hodapp分类)。
主要结果是在24个月时使用视觉功能问卷(VFQ-25)测量的健康相关生活质量。次要结局包括患者报告的结局:EuroQol Group的5维5级健康状况问卷(EQ-5D-5L),健康效用指数标记(HUI-3),青光眼效用指数(GUI),30和病人的经历。
对于VFQ-25,值的范围是从0(代表最低的视觉生活质量)到100(代表最高的视觉生活质量)。对于EQ-5D和HUI-3,得分0等于死亡状态,而1是完全健康状态。对于GUI,就青光眼的影响和治疗的副作用而言,0是最差的状态,而1则是可能的最佳状态。
次要临床疗效结果是眼压,平均分辨力对数(logMAR)视力对数,使用汉弗莱视野分析仪测量的视野平均偏差,白内障手术的需要,驾驶视觉标准的通过/不通过(基于(Esterman视野),视力障碍认证的资格以及干预措施的安全性。
研究分析发现,在24个月时,小梁切除术和医疗管理部门的VFQ-25平均得分分别为85.4(13.8)和84.5(16.3),平均差异为1.06(95%置信区间-1.32至3.43; P = 0.38)。
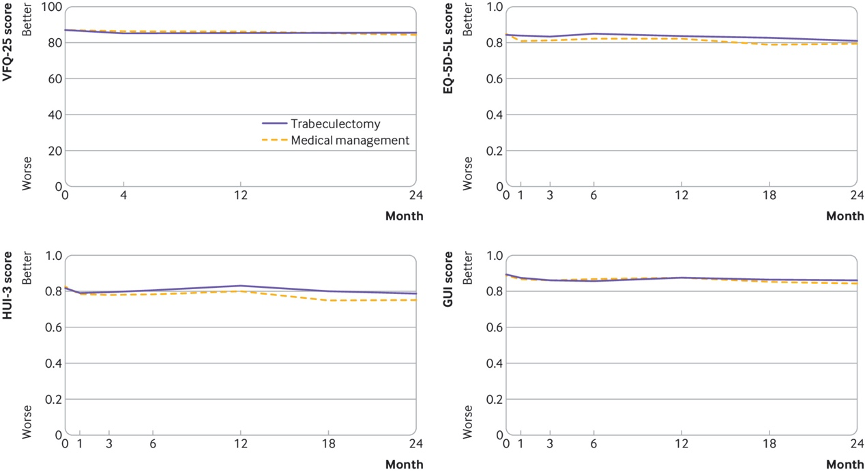
视觉功能问卷
小梁切除术组在24个月时的平均眼内压为12.4mm Hg,医疗管理组为15.1mm Hg(平均差-2.75(95%置信区间-3.84至-1.66)mm Hg; P <0.001)。小梁切除术组的logMAR视敏度更高(更差)(平均差异0.07,0.02至0.11; P = 0.006)。且没有发现在24个月时视野平均偏差(平均差异0.18(-0.58至0.94)dB; P = 0.65)或其他次要结局差异的证据。
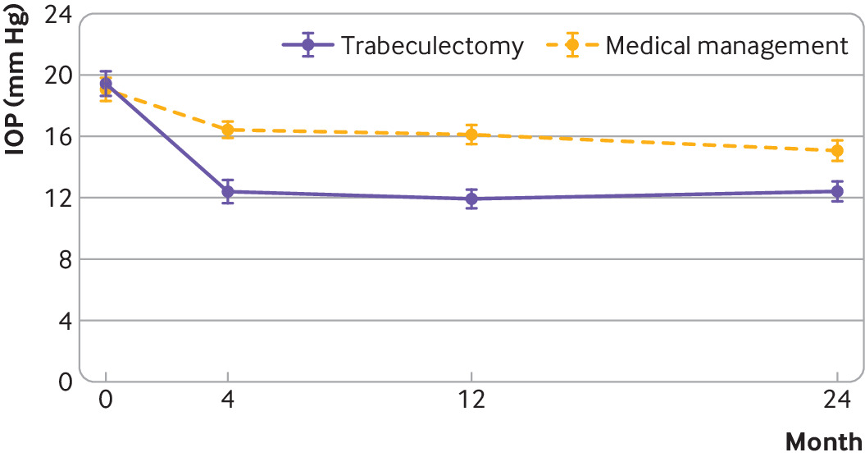
按组别划分的索引眼的平均眼压(IOP)随时间变化情况
研究结果表明,与小剂量药物相比,小梁切除术具有相似的生活质量和安全性,并且眼压更低。
原始出处:
Primary trabeculectomy for advanced glaucoma: pragmatic multicentre randomised controlled trial (TAGS). BMJ 2021; 373 doi: https://doi.org/10.1136/bmj.n1014
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#小梁切除术#
73
视觉功能问卷
76
#BMJ#
67
#小剂量#
66
#切除术#
51
#眼压#
70