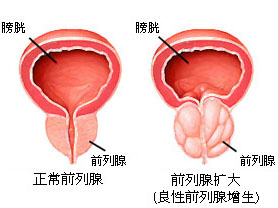
JAMA Surg:2012年后,前列腺活检和切除术在下降
2016-11-09 MedSci MedSci原创
研究表明,USPSTF在2012年提出反对前列腺特异性抗原筛查后,前列腺特异性抗原筛查显著下降。研究目的是确定2012 USPSTF提出的这项建议对前列腺癌诊断与治疗的实践模式的下游效应。研究中的手术记录来自美国泌尿科学委员会,并识别至少进行一次前列腺活检的泌尿科医生(n = 5173)或至少进行一次根治性前列腺切除术(RP)的泌尿科医生(n = 3748)。2012 USPSTF后,每位泌尿科医
研究表明,USPSTF在2012年提出反对前列腺特异性抗原筛查后,前列腺特异性抗原筛查显著下降。
研究目的是确定2012 USPSTF提出的这项建议对前列腺癌诊断与治疗的实践模式的下游效应。
研究中的手术记录来自美国泌尿科学委员会,并识别至少进行一次前列腺活检的泌尿科医生(n = 5173)或至少进行一次根治性前列腺切除术(RP)的泌尿科医生(n = 3748)。
2012 USPSTF后,每位泌尿科医生的前列腺活检中位数下降,从29到21(四分位数范围[IQR}, 12-34; P < .001)。校正混杂因素后,下降幅度为28.7%(参数估计,−0.25; SE, 0.03; P < .001)。
2012 USPSTF后,每位泌尿科医生的RP量中位数从7 (IQR, 3-15)下降到6 (IQR, 2-12) (P < .001),校正混杂因素后,下降幅度为16.2%(参数估计, −0.15; SE, 0.05; P = .003)。
继2012 USPSTF提出后,前列腺活检和RP量明显下降。还需要更多的研究,评价2012 USPSTF的长期后果。
原始出处:
Joshua A. Halpern, MD, MS1; Jonathan E. Shoag, MD1; Amanda S. Artis, MS, MPH2; et alNational Trends in Prostate Biopsy and Radical Prostatectomy Volumes Following the United States Preventative Services Task Force Guidelines Against Prostate-Specific Antigen Screening JAMA Surg. Published online November 2, 2016. doi:10.1001/jamasurg.2016.3987
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#前列腺活检#
80
#切除术#
77
这个翻译好像不够地道啊
86
#活检#
67