郭艺芳:PCI围术期是否需要大剂量他汀治疗?
2015-05-13 郭艺芳 郭艺芳微博
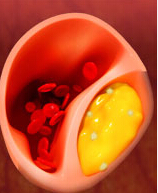
——期待更多证据很多学者认为,冠状动脉疾病介入治疗(PCI)围术期应该予以大剂量他汀治疗,其最经典的证据来自于样本规模较小(共171例患者)、单中心、短期随访(30天)的ARMYDA-ACS研究。由于迄今仍缺乏证据力度更大的多中心随机化临床证据,目前对于PCI围术期的他汀治疗策略仍存在很大争议。2014年发表的由赵水平、霍勇教授等人领导完成的以我国急性冠脉综合征患者为对象的CHILLAS研究(共纳
2014年发表的由赵水平、霍勇教授等人领导完成的以我国急性冠脉综合征患者为对象的CHILLAS研究(共纳入1355例患者,随访期2年)[Atherosclerosis 2014 Apr;233(2):707-12]显示,与常规剂量他汀组(应用10mg/d阿托伐他汀或其他相当剂量的他汀)相比,增加他汀治疗强度(20mg/d阿托伐他汀或其他相当剂量的他汀)并未带来更多获益。这一研究结果提示我们应重新审视我国高危冠心病(急性冠脉综合征或PCI围术期患者)的他汀治疗策略。
新近,在2015年美国心血管造影与介入治疗学会(SCAI)年会期间,公布了以日本患者为基础的MILLION研究结果发现,PCI围术期患者应用较大剂量他汀治疗并未产生更多获益。该研究以100例LDL-C>2.6mmol/L、术前未接受降脂治疗的患者为对象,随机纳入标准治疗组(5mg/d阿托伐他汀和2.5mg/d氮氯地平)或强化治疗组(上述药物药物剂量加倍)。随访18-24个月。观察终点为治疗前后冠状动脉内超声(IVUS)检测的斑块容积。本文不涉及对降压治疗数据的分析。降脂治疗研究数据显示,研究结束时标准治疗组与强化治疗组患者LDL-C水平分别达到1.39mmol/L与1.23mmol/L(两组相差0.16mmol/L,p=0.007)。与治疗前相比,标准治疗组与强化治疗组冠状动脉斑块容积分别降低8.74%与9.37%,均较基线数据显著降低,但治疗后两组间斑块容积无显著差别,两组管腔与血管容量亦无显著差异。实际上,MILLION研究结果不仅在PCI围术期他汀用药剂量方面给我们以启示,与此同时,该研究还表明日本人群使用较低剂量他汀治疗可使多数冠心病患者LDL-C达标。这一发现与我国多数研究结果相一致。
MILLION研究是一项规模较小的替代终点研究,单此一项研究固然不能对临床实践产生影响。但本研究给我们一个重要提示,这就是要充分重视不同人种对相同药物治疗方案的反应可能存在显著不同,在将欧美研究结论运用于亚洲人群时需要慎之又慎。由于以我国人群为基础的临床研究证据尚少,多年来我国临床策略的制定主要参照欧美国家的研究结果。由于不同国家与种族的具体情况(特别是遗传学背景)有显著不同,在一定程度上影响了欧美国家研究结果对我国临床实践的指导价值。换言之,对待欧美国家的研究结论与指南性文件,我们需要借鉴,但要批判性的借鉴,而不是照搬。在我国本土化研究证据尚较少之际,我们既要参考国外研究结果,又要充分考虑我国的流行病学和观察性临床研究结果以及人口学特征与社会经济学背景,以此为基础制定适合于我国国情的疾病防治策略。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










医学约来越细化,讲究证据!
128
不断学习!
130
#围术期#
65
#大剂量#
56
看看
136