BMJ:治疗2型糖尿病,二甲双胍与磺脲类药物联用比单独用药更安全
2018-07-21 佚名 medicalxpress
发表在《英国医学杂志》上的一项研究发现,对于2型糖尿病患者来说,使用磺酰脲类药物来控制血糖水平与使用二甲双胍相比,会增加并发症的风险。
因此,研究人员表示,在引入磺脲类药物时,继续使用二甲双胍比切换更安全。
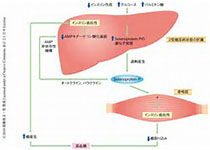
二甲双胍是一种治疗2型糖尿病的“一线”疗法(第一种将要尝试的药物)。但磺脲类药物是最常用的“二线”治疗方法,常与二甲双胍联合使用。
磺脲类药物的安全性已被广泛研究。然而,与单独使用二甲双胍治疗相比,添加或切换到磺脲类药物的具体风险却鲜为人知。
因此,由加拿大麦吉尔大学的萨米·苏伊萨教授领导的一个研究小组,开始评估是否增加或转向磺脲类药物会增加患严重并发症的风险,而在2型糖尿病患者中仅使用二甲双胍的风险就会增加。
他们分析了英国临床实践研究数据链在1998年至2013年间开始二甲双胍治疗的77,000名2型糖尿病患者(平均年龄64岁)的数据。
随后添加或转换到磺脲类药物的患者被识别并与一个单独使用二甲双胍的病人相匹配。
在一年多一点的平均随访期内,使用磺脲类药物(转换和添加联合用药)会增加心脏病发作的风险(每1000人每年7.8 v 6.2次),所有这些都会导致死亡率(27.3 v 21.5次)和严重低血糖(5.5 v 0.7次),而仅仅使用二甲双胍就会增加。
与在二甲双胍治疗中加入磺脲类药物相比,改用磺脲类药物可增加心脏病发作的风险和所有原因的死亡率,但缺血性卒中、心血管死亡或严重低血糖均无差异。
在进一步的分析后,结果仍然相似,以测试结果的强度。
这是一项观察性研究,因此无法确定因果关系,研究人员说,他们不能排除某些观察到的风险可能是由其他未测量的(混杂的)因素造成的可能性。尽管如此,他们说他们的结果是高度一般化的,并且大的样本容量允许计算精确的估计。
因此,他们得出的结论是,磺脲类药物作为二线药物“与二甲双胍单一治疗相比,与增加心肌梗死的风险、所有原因的死亡率和严重的低血糖有关”。
他们补充说,重要的是,与心肌梗死和所有原因死亡的关联“是由使用磺脲类药物而不是添加磺脲类药物引起的”。“因此,按照目前关于治疗2型糖尿病的建议,在引入磺脲类药物时,继续使用二甲双胍比改用二甲双胍更安全。”
美国研究人员Lucy D'Agostino McGowan和Christianne Roumie在一篇相关的社论中说,这一新的证据有助于将治疗决策个性化,并将危害降至最低。
他们指出,很难根据观察性研究来定义临床实践,因为使用不同疗法的患者可能在无法测量的方面存在差异。然而,他们说,这项研究“设计得很好,而且它们之间的关系看起来很牢固和一致。”
drugs in type 2 diabetes and the risk of cardiovascular and hypoglycaemic events: population based cohort study, The BMJ, www.bmj.com/content/362/bmj.k2693
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#BMJ#
44
#磺脲类#
0
#药物联用#
59
谢谢MedSci提供最新的资讯
72
了解一下,谢谢分享!
89
联合用药优点多多。
93