ESC2017重磅研究:RE-DUALPCI研究:房颤患者冠脉介入术后抗凝策略将有重大突破?
2017-08-15 文韬 中国循环杂志
2周后,2017年欧洲心脏病学会(ESC)年会就要召开了,会上将要公布一项万众瞩目的研究:RE-DUALPCI?,该研究的目的是,对于房颤患者,在冠状动脉介入治疗(PCI)术后比较达比加群联合P2Y12抑制剂双抗,是否优于华法林联合双联抗血小板治疗?
2周后,2017年欧洲心脏病学会(ESC)年会就要召开了,会上将要公布一项万众瞩目的研究:RE-DUALPCI?,该研究的目的是,对于房颤患者,在冠状动脉介入治疗(PCI)术后比较达比加群联合P2Y12抑制剂双抗,是否优于华法林联合双联抗血小板治疗?
房颤PCI患者抗凝面临困境
对于接受PCI的患者而言,如果同时有房颤,术后的抗凝就成了问题。因为PCI术后要求使用双联抗血小板治疗,脑卒中高危房颤则需要使用华法林或新型抗凝药物抗凝。同时使用多种抗栓药物就有出血的风险。
之前国内外多项指南的相关推荐,多为华法林与抗血小板药物的双联、三联抗栓治疗。但近年来,随着新型抗凝药物的经验积累,关于新型抗凝药物与华法林用于PCI术后的疗效与安全性比较,已有多项大型随机对照试验。
之前的PIONEER AF-PCI研究发现,利伐沙班在心血管事件减少方面未优于华法林,而是减少了TIMI 大出血/小出血和需要临床关注的出血事件。但其使用的利伐沙班剂量(2.5 mg BID与15/10 mg QD)并未被批准用于房颤患者卒中预防。
2016年欧洲心律协会(EHRA)相关指南指出,在房颤伴冠心病患者中,新型抗凝药物似乎优于华法林。
在这种情况下,RE-DUAL PCI?研究能否成功突围就成了令人瞩目的焦点。
RE-DUAL PCI研究设计
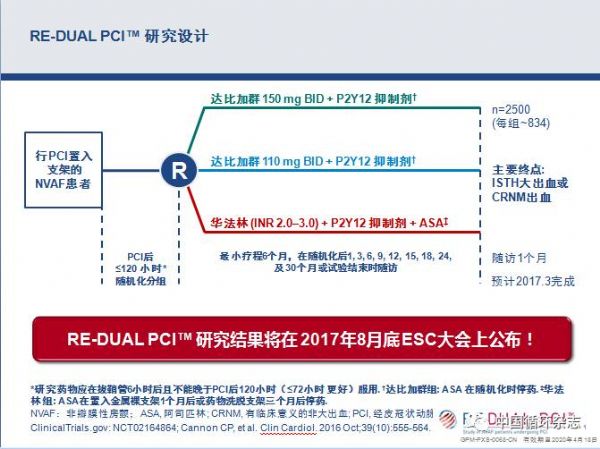
RE-DUAL PCI研究是一项在2502例非瓣膜性房颤冠脉介入患者中进行的全球、事件-驱动、临床Ⅲb期、前瞻性、随机、开放标签,盲终点(PROBE)的活性对照研究,旨在验证达比加群在这类患者中的安全性和疗效。
RE-DUAL PCI研究设计示意图
研究中,受试者被随机分为3组(每组834例),分别接受达比加群(150 mg BID)加一种抗血小板药物 (P2Y12抑制剂)、达比加群(110 mg BID)加一种抗血小板药物(P2Y12抑制剂)和华法林加二联抗血小板药物(阿司匹林+P2Y12抑制剂)治疗。
试验主要终点是评估至首次发生国际血栓与止血学会(ISTH)定义的大出血事件,或主要的临床相关非大出血事件(CRNM)发生的时间。
哈佛大学Christopher Cannon教授是该研究的首席研究者,称该研究将会为接受PCI治疗的房颤患者带来福音。
另外还有两项研究也在进行,分别是AUGUSTUS ACS/PCI(阿哌沙班vs华法林)和ENTRUST-AF-PCI(依度沙班vs华法林)。
原始出处:
[1] Lamberts M, Gislason GH, Lip GY, et al. Antiplatelet therapy for stable coronary artery disease in atrial fibrillation patients taking anoral anticoagulant: a nationwide cohort study. Circulation.
[2] Heidbuchel H, Verhamme P, Alings M,et al. Updated European Heart Rhythm Association practical guide on the use of non-vitamin-K antagonistanticoagulants in patients with non-valvular atrial fibrillation: Executive summary. Eur Heart J.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#ALP#
85
#抗凝策略#
86
#ESC2017#
70
#重磅#
74
#冠脉介入术#
78
#房颤患者#
106