微创治疗先天性肛门闭锁1例
2013-07-25 首都儿科研究所附属儿童医院外科 明安晓 李龙 中国医学论坛报
病历摘要 患儿男,3月21天。因“出生后无肛门,横结肠造瘘后3月余”入院。 患儿出生后无肛门,行倒立位平片检查显示:直肠末端距皮肤44 mm,诊断为高位肛门直肠畸形,遂行横结肠造瘘手术,术后进食好,瘘口排便正常。 入院行瘘口远端注入造影剂,见直肠显影,轻度扩张,造影剂进入膀胱并经尿道流出,诊断为无肛直肠尿道瘘。确诊后第3天行腹腔镜辅助
病历摘要
患儿男,3月21天。因“出生后无肛门,横结肠造瘘后3月余”入院。
患儿出生后无肛门,行倒立位平片检查显示:直肠末端距皮肤44 mm,诊断为高位肛门直肠畸形,遂行横结肠造瘘手术,术后进食好,瘘口排便正常。
入院行瘘口远端注入造影剂,见直肠显影,轻度扩张,造影剂进入膀胱并经尿道流出,诊断为无肛直肠尿道瘘。确诊后第3天行腹腔镜辅助肛门直肠成形术。
手术过程 患儿取平卧位,于脐及左右下腹置入3个5 mm 套管。镜下游离直肠远端至直肠尿道瘘管处,距尿道前列腺部0.5 cm 开始沿远端直肠的黏膜下层剥离,彻底切除瘘管黏膜,保留肌层(图1)。以5-0 PDS可吸收线横行连续缝合瘘管肌层,缝合确切,无张力(图2)。从盆腔侧,沿左右耻骨尾骨肌的中缝游离约1.0 cm深(图3)。游离直肠,在肠系膜根处离断直肠上动脉,使直肠近端达到盆底水平。转截石位,在电刺激仪的帮助下寻找肌肉收缩中心,沿肌肉中心向上分离1.5 cm以后(图4),在腹腔镜监视下贯通盆腔侧隧道,将直肠沿隧道拖出至会阴部(图5),检查血运,在无张力的情况下将直肠末端与会阴部皮肤相吻合(图6)。

图1 游离直肠远端,切除直肠尿道瘘

图2 可吸收线缝合关闭瘘管肌层
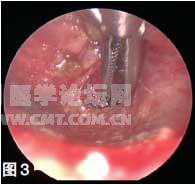
图3 从盆腔侧沿肌肉中心分离耻骨直肠肌

图4 在会阴部沿肌肉收缩中心向上分离

图5 腹腔镜下将直肠沿隧道拖出至会阴部

图6 将直肠末端与会阴部皮肤吻合
讨论
高位肛门直肠畸形的治疗一直被小儿外科医师关注,随着手术技术的改进,该先天畸形的治疗水平已有很大提高。但由于患儿盆底肌及神经往往发育不良,这使得在肛门直肠成形术中减少对盆底肌肉及神经的损失显得尤为重要。
2000年,乔治森(Georgeson)等提出腹腔镜辅助肛门直肠畸形成型术(LAARP)。腹腔镜手术的优越性在于,① 可以更容易地分离直肠末端和直肠尿道或直肠阴道瘘管,处理瘘管更加确切,避免损伤尿道。由于可以更充分地游离直肠,所以LAARP手术时不管有没有前期的结肠造瘘,均不会出现拖出肠段过短、张力增高的问题。② 由于腹腔镜具有放大功能,可以从盆腔看到两侧的耻骨尾骨肌肌腹,同时配合电刺激准确辨认肌肉的收缩中心,指导直肠从盆底拖出的隧道位于肌肉中心,减少对括约肌复合体的损伤,避免了开放手术中括约肌复合体的瘢痕愈合,使术后便秘发生率显著降低。③ 术后肠功能恢复快、进食早、住院时间短、创伤小。
尽管尚无腹腔镜治疗高位肛门直肠畸形疗效的长期评估报告,但中期随访结果显示,约70%的患儿在手术3年后可以获得满意的排便控制功能,这与传统的后矢状入路手术并无明显差异;但随访中很少见到术后便秘的病例,这体现了腹腔镜微创在该手术中的优势。由于该技术开展时间仍然较短,仍需要更长期的随访以对其疗效做出进一步分析。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#微创治疗#
64
#肛门#
53
#微创#
62
#先天性#
56