Lancet Oncol:采用单次术中放疗的早期乳腺癌的长期(15年)预后
2021-04-21 Nebula MedSci原创
对于早期乳腺癌患者,单次术中放疗 pk 术后分次全乳放疗的长期预后,孰优孰劣?
放疗继续在早期乳腺癌的治疗中发挥着重要作用,可降低患者的总体复发率和死亡率。既往关于术中电子线放疗(ELIOT)的随机3期等效试验显示,对于早期乳腺癌患者,相比全乳放疗(WBI),采用术中放疗的加速局部乳腺放疗(APBI)与同侧乳腺肿瘤复发率(IBTR)更高相关。
近日发表在柳叶刀子刊“Lancet Oncology”上的一篇文章“Intraoperative irradiation for early breast cancer (ELIOT): long-term recurrence and survival outcomes from a single-centre, randomised, phase 3 equivalence trial”,评估了ELIOT试验患者的长期复发率和生存预后。
ELIOT试验是一项在意大利开展的单中心、随机的3期试验,招募了48-75岁的临床确诊的单中心性乳腺癌患者,且要求肿瘤直径不超过25mm、无淋巴结转移、可进行保乳手术治疗。受试患者按1:1倍随机分至两组,接受术后常规分次的WBI(50 Gy,分25次)或单次术中21 Gy的电子线放疗(ELIOT)。主要终点是IBTR的发生率。次要终点是总体存活率。
2000年11月20日-2007年12月27日,共招募了1305位患者,其中654位被分至WBI组,651位被分至ELIOT组。
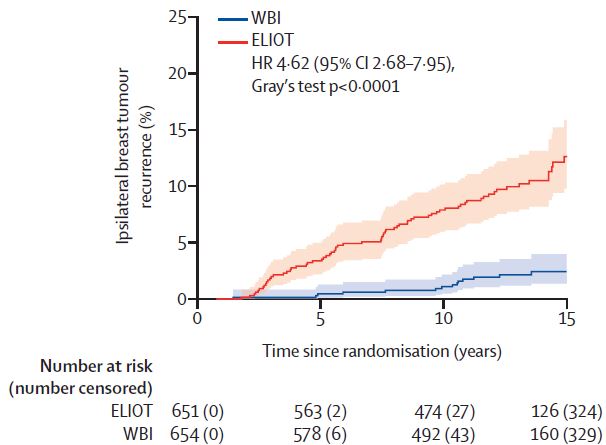
两组的累积IBTR发生率
中位随访了12.4年(IQR 9.7-14.7)后,有86位(7%)患者发生了IBTR,其中70例(11%)是在ELIOT组,16例(2%)是在WBI组,对应的ELIOT组有54例绝对过量的IBTR(HR 4.62,95%CI 2.68-7.95,p<0.0001)。在ELIOT组,5年IBTR率为4.2%(95%CI 2.8-5.9),10年IBTR率为8.1%(6.1-10.3),15年IBTR率为12.6%(9.8-15.9)。在WBI组,5年IBTR率为0.5%(95%CI 0.1-1.3),10年IBTR率为1.1%(0.5-2.2),15年IBTR率为2.4%(1.4-4.0)。
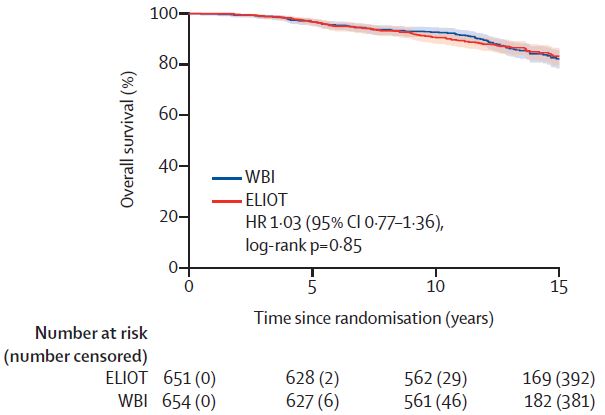
截止2019年3月11日最后一次随访,共有193位(15%)女性死亡(死因不限),两组间的死亡率无明显差异(ELIOT组 98例 vs WBI组 95例;HR 1.03, 95%CI 0.77-1.36, p=0.85)。
两组的总体存活率
在ELIOT组,5年、10年和15年时的总体存活率分别为96.8%、90.7%和83.4%;在WBI组,相应的总存活率分别为96.8%、92.7%和82.4%。
综上所述,该试验的长期结果证实,ELIOT组的IBTR率明显高于WBI组,但总存活率无明显差异。低IBTR组的患者或许可以选用ELIOT。
原始出处:
Orecchia Roberto,Veronesi Umberto,Maisonneuve Patrick et al. Intraoperative irradiation for early breast cancer (ELIOT): long-term recurrence and survival outcomes from a single-centre, randomised, phase 3 equivalence trial. Lancet Oncol, 2021, https://doi.org/10.1016/S1470-2045(21)00080-2
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Lancet#
64
#Oncol#
0
放疗与同侧乳腺肿瘤复发率
88
顶刊就是不一样,质量很高,内容精彩!学到很多
83
谢谢梅斯分享这么多精彩信息
79