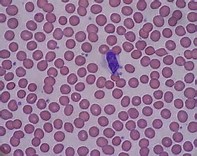
Blood:急性血小板减少后,新产生的幼稚血小板常出现GPVI信号缺陷。
2018-01-03 MedSci MedSci原创
血管损伤的部位,暴露的内皮下胶原通过与血小板表面的免疫受体酪氨酸激活模体(ITAM)-偶联糖蛋白(GP)VI相互作用,,从而激活血小板和血栓形成。血小板是由巨核细胞(MKs)的细胞质衍生而来,巨噬细胞将巨大的血小板前体延伸到骨髓(BM)窦,进而脱落入血,最终在血液中形成正常大小的血小板并成熟。在胶原蛋白富集的BM环境中,MKs活化以及形成血小板前体的过程受抑制的机制仍不明确。本研究中,研究人员发现
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#GPVI#
66
学习一下很不错
107
学习了谢谢作者分享!
114
#血小板减少#
62
学习了很有用
116
谢谢分享.学习了
101
学习一下谢谢
106