JACC:冠脉微血管功能不良可作为肥胖患者的心血管风险分层因子
2018-08-08 MedSci MedSci原创
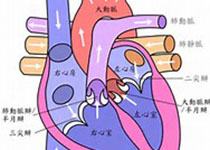
除了体重指数(BMI)外,尚需要其他的因素来鉴别肥胖患者的心血管风险。本研究的目的旨在评估肥胖、冠脉微血管功能不良(CMD)和不良反应事件的相关性。本研究对827名心脏灌注正电子发射断层显像显示正常灌注的肥胖患者进行平均5.6年时间的随访,观察事件主要包括死亡、心梗或心衰住院。分析结果显示,BMI与冠脉血流储备(CFR)呈倒J型曲线相关,即在肥胖患者中,CFR随着BMI的升高而降低(p <
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#JACC#
61
#血管风险#
54
#冠脉微血管功能#
86
#肥胖患者#
56
#ACC#
63
#风险分层#
81
#微血管#
80
#血管功能#
56