Cell:重大发现!lincRNA-EPS抑制炎症产生
2016-07-17 生物谷 生物谷
在一项新的研究中,来自美国马萨诸塞大学医学院的研究人员鉴定出一种被称作lincRNA-EPS的长链非编码RNA(lincRNA)负责调节先天免疫。lincRNA-EPS是在巨噬细胞中大量发现的,在遭遇病原体之前,一直让触发炎症的基因处于关闭状态。这一发现指出lincRNA在免疫系统中的一个未被识别的作用,可能对不受控制的免疫反应(如狼疮或炎症性肠病)导致的炎性疾病产生新的认识。相关研究结果近期发表
论文通信作者、马萨诸塞大学医学院医学教授Katherine A Fitzgerald博士说,“这些发现提示着存在一层未被研究的控制炎性反应和免疫反应的调控。我们证实一种lincRNA在免疫系统中发挥重要的作用。”
长链非编码RNA(lincRNA)是非编码蛋白的转录本,它们的长度大于200个核苷酸(从而有助将它们与微RNA、小干扰RNA、piRNA和其他短链RNA区分开来)。人们认为lincRNA可能占人类基因组的RNA转录本中的绝大多数。Fitzgerald说,“尽管它们大量存在,但是很少有人了解这些长链RNA在免疫系统中的功能。为了试图了解控制免疫系统的复杂基因通路,免疫学家历来集中关注编码蛋白的基因(占基因组的2%)。”
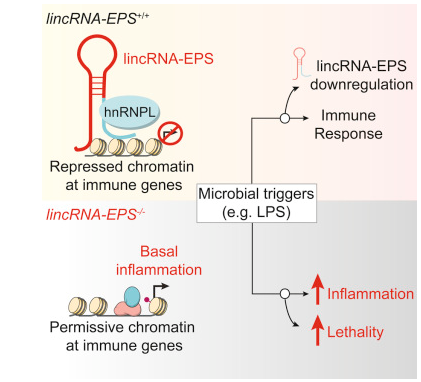
利用一种缺乏lincRNA-EPS的模式小鼠,Fitzgerald和同事们证实在正常状态下,巨噬细胞(一类抵抗感染的白细胞)产生lincRNA-EPS来阻止免疫反应基因自动激活。然而,当巨噬细胞检测到潜在的病原体时,lincRNA-EPS表达受到抑制,不再阻止免疫反应基因激活,因而启动促炎反应。缺乏lincRNA-EPS的小鼠产生水平增加的细胞因子和炎性反应,从而导致中毒性休克。
研究人员发现,lincRNA-EPS控制核小体的位置而使得它们难以接近,从而持续抑制免疫反应基因表达。当lincRNA-EPS不再在巨噬细胞中表达时,基因组结构发生变化,因而关键性的免疫相关基因被暴露出来。当研究人员再次将lincRNA-EPS导入这些细胞中时,免疫相关基因表达恢复到正常水平。
论文第一作者、马萨诸塞大学医学院博士后研究员Maninjay K. Atianand博士说,“我们还发现,lincRNA-EPS本身的表达受到非常严格地调控,对微小的变化非常敏感。这种lincRNA是阻止关键性免疫基因自动激活的分子通路中的一种重要组分。这些发现对lincRNA可能在慢性炎症和免疫病理学中发挥着的潜在作用产生重要影响。”
Fitzgerald和同事们的下一步是确定lincRNA-EPS在肠道炎症中发挥着什么作用,以及它在结肠中的功能,这是因为已发现它在结肠中大量存在。
小编向大家推荐一个学术会议,不要错过哦:2016癌症、炎症与免疫--微环境下的对话
原始出处
Maninjay K. Atianand, Wenqian Hu6, Ansuman T. Satpathy, Ying Shen, Emiliano P. Ricci7, Juan R. Alvarez-Dominguez, Ankit Bhatta, Stefan A. Schattgen, Jason D. McGowan, Juliana Blin, Joerg E. Braun, Pallavi Gandhi, Melissa J. Moore, Howard Y. Chang, Harvey F. Lodish, Daniel R. Caffrey, Katherine A. Fitzgerald.A Long Noncoding RNA lincRNA-EPS Acts as a Transcriptional Brake to Restrain Inflammation.Cell.2016
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#CEL#
96
#lincRNA#
67
#EPS#
101
#Cell#
96
#CRN#
70
#重大发现#
58
溃疡性结肠炎研究中!
147