 news-medical.net
news-medical.net
近年来,全球甲状腺癌发病率不断走高。甲状腺结节出现在越来越多人的体检报告上,“甲状腺癌将被剔除出重大疾病”的说法也多次在社交媒体刷屏。与此同时,对于这种“懒癌”过度诊断的风险也在持续引起关注。过度诊断意味着,一些亚临床疾病,如果没有通过检测手段发现,并不会引起明显的临床症状。
近期,法国里昂国际癌症研究机构(IARC)癌症监测处的专家调查了横跨25个国家/地区按组织学分类的甲状腺癌发病率趋势,数据显示甲状腺癌尤其是乳头状亚型癌发病率近年迅速升高,分析是由于对于该疾病的过度筛查引起。由此,专家目前不建议进行过度的甲状腺癌筛查,因为这可能会在不改善结果的情况下增加患者危害的风险。该研究结果于2021年3月1日发表在《柳叶刀糖尿病和内分泌学》(The Lancet Diabetes and Endocrinology)上。
 Thyroid cancer incidence trends by histology in 25 countries: a population-based study.The Lancet Diabetes and Endocrinology.March 01, 2021.DOI:https://doi.org/10.1016/S2213-8587(21)00027-9
Thyroid cancer incidence trends by histology in 25 countries: a population-based study.The Lancet Diabetes and Endocrinology.March 01, 2021.DOI:https://doi.org/10.1016/S2213-8587(21)00027-9
甲状腺癌包括一系列组织学亚型,占全球癌症诊断的3%。据估计,2020年有58.6万被诊断为甲状腺癌的患者。
近年的证据表明,在过去30年中,许多高收入和中等收入国家的发病率大幅上升,尽管不同地区人口间存在很大差异,而甲状腺癌的死亡率有所下降或基本保持稳定。
为了进一步研究这个问题,研究人员研究了世界卫生组织国际癌症研究机构(IARC)整理的1998-2012年期间的甲状腺癌发病率数据。他们重点研究了来自欧洲、美洲、亚洲和大洋洲的25个国家,这些国家的癌症登记册覆盖了其200多万人口。研究纳入人群年龄在20岁-84岁,且未明确的甲状腺癌病例比例必须低于10%。最终研究共纳入了近15万例甲状腺癌的数据。
在所有国家中,甲状腺乳头状癌是甲状腺癌新发病例的主要类型。尽管各国之间差异很大,但它是所有国家中唯一发病率上升的组织学亚型。2008-2012年期间,女性甲状腺乳头状癌的年龄标准化发病率从荷兰、联合王国和丹麦的每10万人年4.3至5.3例到韩国的每10万人年143.3例不等。在男性中,年龄标准化的发病率从泰国、保加利亚和荷兰的每10万人年1.2至1.6例到韩国的每10万人年30.7例不等。研究期间,女性发病率的增长速度很快,在一些国家超过了每10万人中20例,其中以韩国最为明显。
有趣的是,韩国、中国、日本、土耳其的发病率在2000年代之前一直处于低位稳定,随后明显上升,而美国、奥地利、克罗地亚、德国、斯洛文尼亚、西班牙、立陶宛、保加利亚的发病率增长在2009年前后趋于稳定。
但对于甲状腺癌的其他组织学亚型,发病率的趋势相对稳定且保持在较低水平。
美国、中国、韩国、土耳其等一些国家和一些北欧国家的滤泡状甲状腺癌的发病率有所上升,但比乳头状甲状腺癌的发病率低得多。总的来说,年龄标准化的甲状腺滤泡癌发病率在女性中为每10万人年0.5~2.5,在男性中为每10万人年0.3~1.5。甲状腺髓质癌的发病率在男性和女性中均低于每10万人中1人。对于无细胞亚型,比率低于每10万人年0.2个。同时,在研究期间,21个国家中的甲状腺非典型性癌的发病率都有小幅下降。
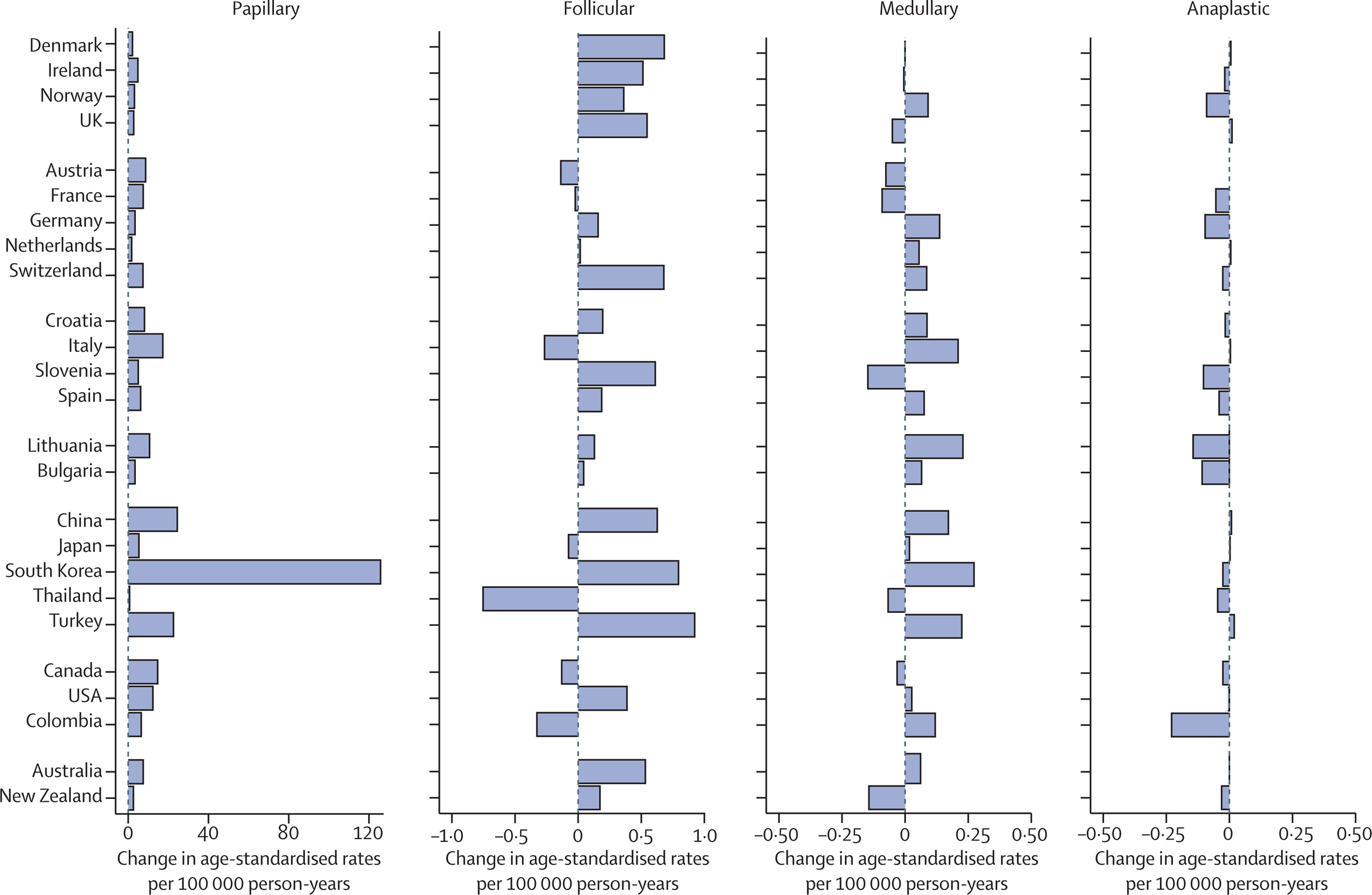 按不同类型不同地区甲状腺癌发病率变化
按不同类型不同地区甲状腺癌发病率变化
研究表明,在1998年至2012年期间观察到的甲状腺癌发病率的快速增加在很大程度上限于乳头状甲状腺癌,这种亚型更多以亚临床形式被发现。
乳头状癌(PTC)是最常见的分化良好的甲状腺癌,也是最常见的由放射线引起的甲状腺癌。通常是通过对甲状腺的严格筛查来发现。这些患者中绝大部分接受甲状腺全切术,有相当比例的患者同时接受颈部淋巴结清扫术和放射治疗。但有研究显示,这些干预并未证实在改善患者生存上显示获益。这一发现在国际上阐明了甲状腺癌过度诊断的流行病学特征,并进一步证实了过度诊断在观察到的甲状腺癌发病率增加中的驱动作用。
甲状腺癌过度诊断与医疗监测的增加及诊断技术的不断引入相关,如颈部超声检查(自上世纪80年代)及CT扫描和MRI。这些技术的引进使得甲状腺内的大量惰性、非致命性疾病得到诊断,而这些疾病引起症状或导致死亡的可能性很小。
自从超声诊断引入后,一些国家如美国、意大利和法国甲状腺癌诊断受到的影响较大。不过最引人注目的还是韩国。根据最近几年数据,超声引入后甲状腺癌已经成为韩国女性最常见的癌症诊断。
世界范围内,甲状腺癌的过度诊断症正逐渐增加,伴随而来的是一些不必要手术的增加。研究数据这为某些类型的甲状腺乳头状癌应重新归类为良性肿瘤的建议提供了证据。
2016年,由病理学家和临床医生组成的国际专家小组对非侵袭性、复发风险较低的甲状腺癌进行了重新分类。专家小组将滤泡型甲状腺乳头状癌(EFVPTC)更名为以乳头状核为特点的非侵袭性滤泡型甲状腺肿瘤(NIFTP)。
随后,ATA指南在2016年发布的更新版指南指出甲状腺叶切除术为分化良好的甲状腺癌的一项替代治疗。关于何时进行甲状腺结节活检,遵循ATA指南可以减少过度诊断的发生。
2019年12月,澳大利亚的一项研究分析了30多年的国家医疗数据,得出结论:五种最常见的癌症(乳腺癌、甲状腺癌、肾癌、前列腺癌和黑色素瘤)中约有20%是“过度诊断”的结果。该研究在线发表在《澳大利亚医学杂志》上。
研究显示,在研究期间的女性中有22%的乳腺癌(包括13%的浸润性病例)、58%的肾癌、73%的甲状腺癌和54%的黑色素瘤(包括15%的浸润性病例)被过度诊断。这相当于女性这五种癌症诊断总数的18%(占侵袭性癌症的8%)。
在男性中,有42%的前列腺癌、42%的肾癌、73%的甲状腺癌和58%的黑色素瘤被过度诊断。这相当于男性这五种癌症所有诊断的24%(占侵袭性癌症的16%)。
 2012年澳大利亚妇女癌症过度诊断的估计数量。Estimating the magnitude of cancer overdiagnosis in Australia.DOI: https://doi.org/10.5694/mja2.50455
2012年澳大利亚妇女癌症过度诊断的估计数量。Estimating the magnitude of cancer overdiagnosis in Australia.DOI: https://doi.org/10.5694/mja2.50455
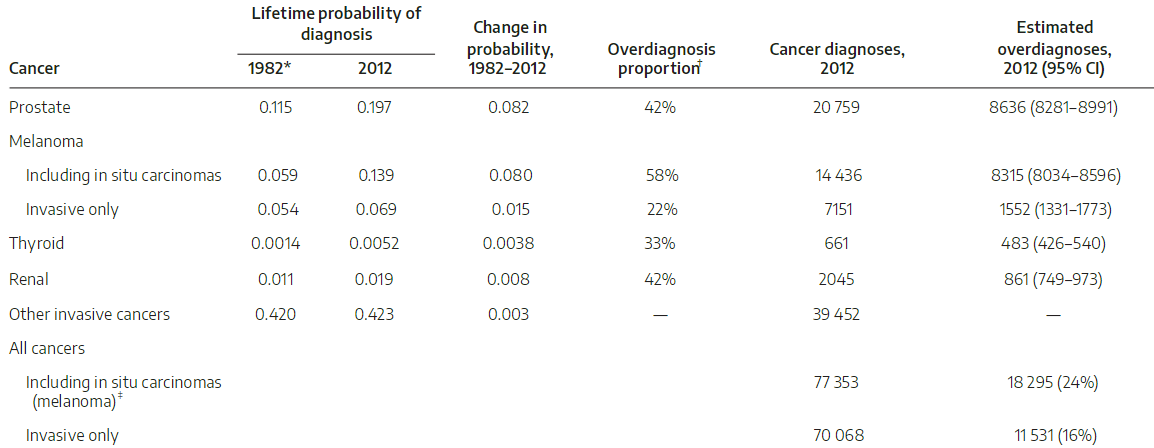 2012年澳大利亚男性癌症过度诊断的估计数量。Estimating the magnitude of cancer overdiagnosis in Australia.DOI: https://doi.org/10.5694/mja2.50455
2012年澳大利亚男性癌症过度诊断的估计数量。Estimating the magnitude of cancer overdiagnosis in Australia.DOI: https://doi.org/10.5694/mja2.50455
在对结果的讨论中,研究团队指出,英国最近的癌症统计数据显示,1期乳腺癌的5年生存率为99%,1期前列腺癌为100%,1期黑色素瘤为100%,1期肾癌为89%,任何阶段的甲状腺癌为88%。这些非常高的生存率提供了可能是过度诊断的进一步证据。
当涉及到癌症的早期检测时,人们仍然需要保持警惕,然而他们需要了解并与他们的医疗专业人员一起参与关于癌症筛查和其他相关程序的危害的共同决策。
过去十年来,医学界已经做出大量努力来减少对甲状腺乳头状癌的过度诊断,并尽量避免过度治疗。
主流的甲状腺结节和甲状腺癌指南已经更新指出,无需对<1 cm的甲状腺结节进行活检以评估癌症;对于小体积肿瘤,推荐甲状腺半切而非全切手术。放射科相关指南也提出,对于横截面成像检测到的甲状腺偶发结节,减少过度检查;建议根据外观以及尺寸对结节进行分类以指导是否需要后续活检。
为此,包括Mayo Clinic和纪念斯隆-凯特琳癌症中心在内的全球多家顶级医院,以及不少指南目前已经建议,不要在无症状的个体中筛查甲状腺癌,并提倡对微小肿瘤进行积极监测而非立即治疗。
未来,我们需要更好的方法来确定,究竟哪些甲状腺结节有必要进行活检。一些结果不确定的甲状腺活检经常导致甲状腺切除,而最终病理结果又通常是良性的。同时,我们也需要更好地识别,究竟哪些甲状腺癌必须切除。
无论如何,过去十年来,在甲状腺癌诊疗手段进步的同时,过度诊断的现象也已经得到了公认。持续的监测、分析和探讨,将有助于我们更好地发现、更合理地应对甲状腺癌。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#发病率#
64
同感
90
#癌发病#
70
#癌发病率#
103
很好
101
了解
124
好文章!
111
了解
114
好文章!
120