Blood:血小板生成素受体激动剂在ITP老年患者中的实际应用情况
2021-08-26 Nebula MedSci原创
TRA是ITP老年患者的一种有效疗法,且无致命性出血风险,相当一部分患者在停药后仍可保持持续缓解
原发性免疫性血小板减少症(ITP)是一种罕见的获得性免疫疾病,特征是血小板计数<100×109/L和出血风险增加。ITP好发于两个年龄段的患者:儿童和老年人。在老年人中,ITP的发病率随着年龄的增长而进一步升高:60-75岁,发病率为1.94-4.62/10万人;>75岁,发病率为9.0/10万人。
但是,血小板生成素受体激动剂(TRA)在ITP老年患者中的有效性和安全性尚不清楚。ELDERLY-ITP-TRA研究是一项观察性回顾性研究,在384位60岁及以上的ITP患者中评估了TRA的反应性和换药、血栓/出血风险和停止治疗后的持续缓解(SROT)。
多因素分析与TRA治疗失败的风险因素
持续治疗3个月后,采用艾曲波帕(n=271)和罗米司亭(n=113)做一线治疗的患者分别有82.5%和74.3%的获得了缓解。中位随访了2.7年后,截止最后一次随访,仍有66.7%的患者处于缓解中。85位(22.2%)患者改用替代的TRA;虽然未观察到交叉毒性,但83.3%的耐药患者在换药后有所缓解。
18位患者共发生了34例重大血栓事件,其中3例为致命性的;10位患者共发生了14例重大出血,无致命性的;这两种不良事件分别与TRA治疗开始时的血栓病史(风险比[HR] 2.04,p=0.05)和血小板计数<20×109/L(HR 1.69, p=0.04)相关。15.6%的发生过血栓事件的存活患者复发血栓事件,除1例外,所有复发事件都是发生在TRA持续治疗期间(发生率 7.7/100人·年)。所有复发血栓事件都是发生在充分的抗血栓二级预防的缺席情况下。
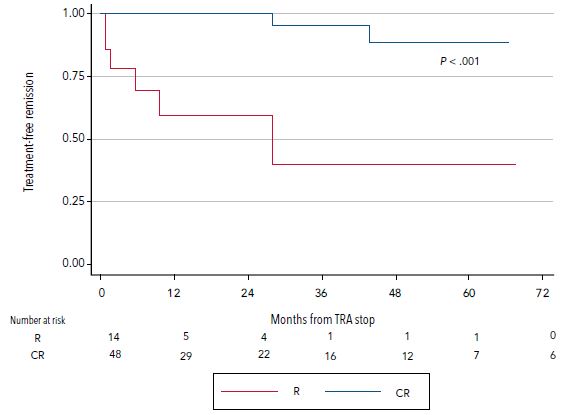
在不同缓解状态下的患者停用TRA后的无治疗缓解期
62位(16.5%)缓解患者停用了TRA,其中53位(13.8%)在停药后维持缓解,这与患者停用TRA时是否是完全缓解相关。高龄(≥75岁,41.1%)与持续/急性期更频繁地开始应用TRA有关,但与缓解或血栓/出血风险无关 。
综上,TRA是ITP老年患者的一种有效疗法,且无致命性出血风险,相当一部分患者在停药后仍可保持持续缓解。此外,既往有血栓病史的患者需谨慎,应注意充分平衡好TRA干预治疗的风险和获益。
原始出处:
Francesca Palandri, et al. Real-world use of thrombopoietin receptor agonists in older patients with primary immune thrombocytopenia. Blood (2021) 138 (7): 571–583. https://doi.org/10.1182/blood.2021010735
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#血小板生成素受体激动剂#
80
#ITP#
99
#激动剂#
75
学习
107
很好的文章
105