spine:维生素D缺乏增加PKP术后椎体再骨折发生风险
2012-08-23 紫川秀第二 丁香园
老年人的椎体压缩性骨折发生率较高,发生椎体压缩性骨折后往往会降低病人的生活质量。椎体成形术出现之前,这类病人往往都采取保守治疗,需要绝对的卧床休息,因而病死率较高。随着微创化手术技术的进展,椎体成形术开始成为老年人骨质疏松性椎体压缩骨折的常用术式。椎体成形术具有创伤小,操作相对简便,对病人的要求较低,在局麻下即可完成等优点。手术后患者疼痛可以立刻缓解,并在术后
老年人的椎体压缩性骨折发生率较高,发生椎体压缩性骨折后往往会降低病人的生活质量。椎体成形术出现之前,这类病人往往都采取保守治疗,需要绝对的卧床休息,因而病死率较高。随着微创化手术技术的进展,椎体成形术开始成为老年人骨质疏松性椎体压缩骨折的常用术式。椎体成形术具有创伤小,操作相对简便,对病人的要求较低,在局麻下即可完成等优点。手术后患者疼痛可以立刻缓解,并在术后1-2天内即可下床负重行走。但事实上关于椎体成形术治疗的手术适应症还存在争议。
已有多项研究表明,椎体成形术后脊柱节段的再骨折率较正常人群有所上升。目前认为原因是多方面的:骨水泥填充的椎体其骨质硬度的改变可能会对整个脊柱力学负荷产生影响,从而导致椎体骨折的加剧发生;术后患者疼痛缓解,重新进行原强度的生活也会造成骨折的再发生;骨质疏松病人病情持续进展也可能造成再骨折发生,但目前对椎体成形术后再发骨折的病人的骨代谢动力学研究较少,血液中各种矿物质和必要维生素的缺乏对术后骨折再发的影响尚未见诸报端,来自希腊的学者就上述问题进行了相关研究,论文发表在spine上。
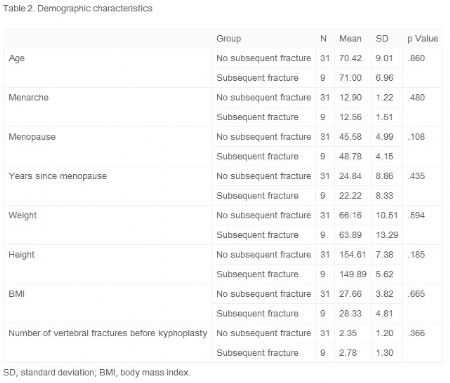
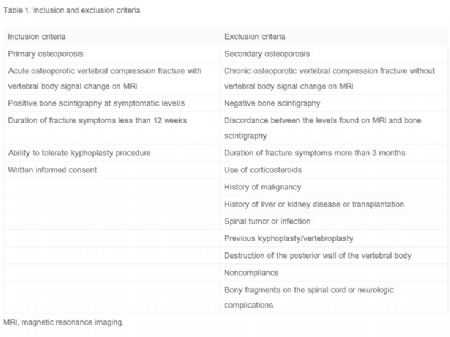
研究者选取40位诊断为骨质疏松伴椎体压缩性骨折的绝经期女性,共进行了98次后凸成形术(人口统计学数据见表1-2)。将纳入研究者分类成为两个组别:再骨折组和未再骨折组(图1)。研究纳入和排除的标准见表3,研究流程见图2。
表2:人口统计学数据(二)

表3:研究纳入排除标准
图1:骨折椎体的节段分布
图2:研究流程图
对纳入研究的患者进行相关指标的统计:年龄,BMI,吸烟史,最初开始的椎体骨折节段,手术中的造影剂渗漏,既往非脊柱部位的骨折,抗骨质疏松治疗,骨密度,骨代谢指标(钙,磷,PTH,肌酐,I型前胶原氨基端肽(PINP),NTx),25羟维生素 D水平等。
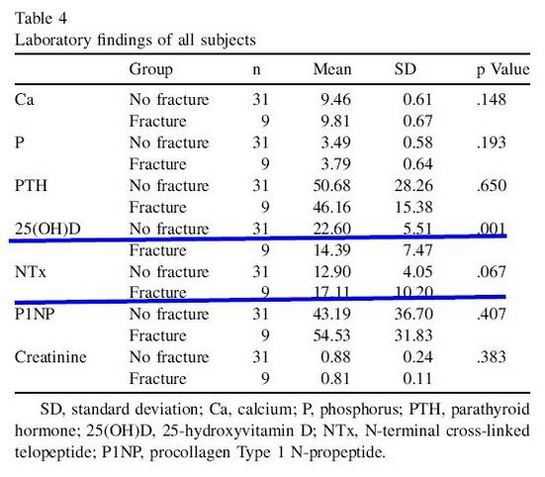
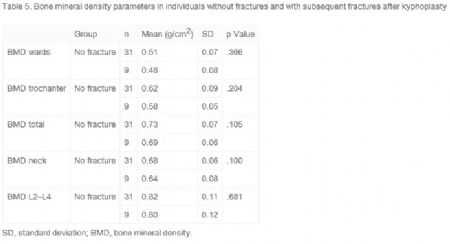
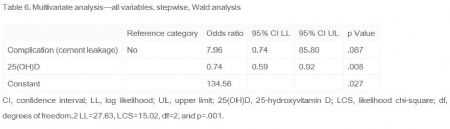
统计结果如表4-6所示。
其中25羟维生素 D水平,再骨折组显着低于未再骨折组,而NTx虽然没有显着性差异,但存在再骨折组比未再骨折组要稍高的趋势。其余指标比较,组间无显着差异。
表4:实验室检查数据组间比较
研究者认为维生素D在骨折重塑过程中发挥着重要的作用,缺乏维生素D会造成骨内微环境的不稳定,延缓骨质矿物化,从而影响骨质的重塑。骨质重塑的延缓可以减弱骨小梁的强度,引发再骨折。所以对骨折病人术后一定要注意抗骨质疏松治疗,补充相关矿物质,椎体成形术只能治标,不能治本,疾病的治疗关键在于预防。
原文链接:
Zafeiris CP, Lyritis GP, Papaioannou NA, Gratsias PE, Galanos A, Chatziioannou SN, Pneumaticos SG. Hypovitaminosis D as a risk factor of subsequent vertebral fractures after kyphoplasty. Spine J. 2012 Apr;12(4):304-12.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Spine#
71
#PKP术后#
52
#椎体#
61