JACC:临床指南更新换代,还不快点给自己充电更新知识库?
2015-07-01 张旭栋 译 MedSci原创
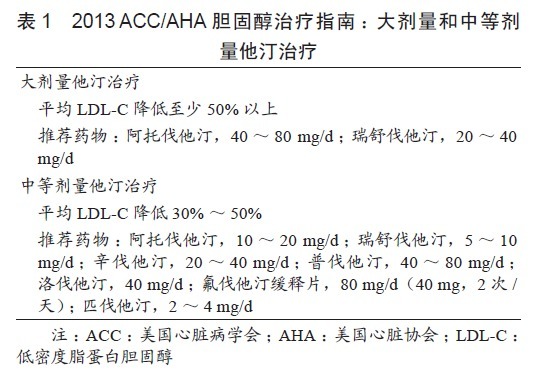
背景:美国心脏病学会(ACC)和美国心脏协会(AHA)一直致力于临床指南的发展,从而帮助临床医生更有效的进行实践操作。目的: 本项研究旨在评估2008年至2014年之间ACC/AHA指南建议的变化。方法:对2008年至2014年间更新的ACC/ AHA指南进行了比较,从而评估新旧指南级别(Class of Recommendation ——COR)和证据水平(Level of Evide
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#临床指南#
50
#JACC#
46
#指南更新#
45
看看
59
#ACC#
38
不错,又有新东西了!
87
压力
105
知识的更新越来越快,有压力呀
109
每次都看
123