Nature:肠道菌引酒精诱发致命肝病“魔高一尺”,噬菌体疗法“道高一丈”!
2019-11-16 佚名 中国生物技术网
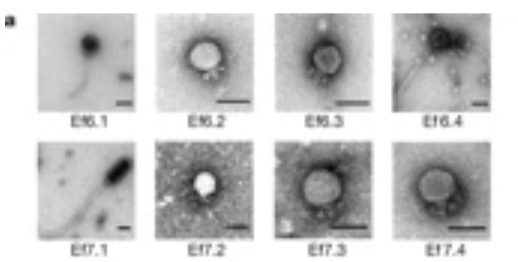
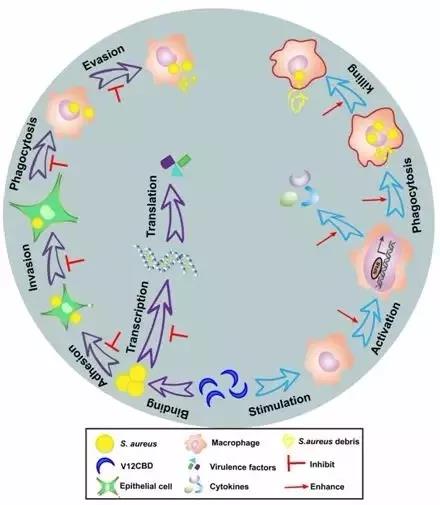
北京时间11月14日,发表在《Nature》上的一项新研究中,来自美国加州大学圣地亚哥分校(UCSD)医学院的研究人员首次将噬菌体疗法应用于小鼠,成功治疗其酒精性肝病。噬菌体是一种专门破坏细菌的病毒。在20世纪初,研究人员曾尝试用噬菌体作为一种治疗细菌感染的潜在方法。但后来由于抗生素的出现,噬菌体不再受关注。如今,随着抗生素耐药性的不断增加,噬菌体疗法又重出江湖。研究通讯作者、医学和胃肠病学教授、

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Nat#
0
#噬菌体#
50
#肠道菌#
53
学习了很有用不錯
87
好好好好好好
93