JCEM:孕晚期孕妇睾酮浓度和子女5岁时握力的关系
2022-03-13 MedSci原创 MedSci原创
妊娠晚期FT浓度与子女5岁时HGS评估的肌肉力量呈负相关,这可能表明母体FT对子代肌肉力量存在负面的影响。
儿童的肌肉力量、爆发力和耐力与性别、年龄、青春期、体育锻炼、骨骼健康和自尊等因素呈正相关;这些肌肉参数与儿童和青少年的肥胖、代谢危险因素和后来的心血管疾病呈负相关。事实上,青春期肌肉力量低下会增加成年早期死亡的风险。有研究报道妊娠期间的母体睾酮水平可能对子代肌肉力量有调节作用。

近日,内分泌和代谢性疾病领域权威杂志Journal of Clinical Endocrinology & Metabolism上发表了一篇研究文章,该研究旨在调查妊娠中期母体睾酮浓度与子代5岁时握力(HGS)之间可能存在的关联。

在基于人群的前瞻性欧登塞儿童队列中,研究人员测量了1017对母子27-28孕周时总睾酮(TT)和子女5岁时的HGS。TT通过液相色谱-串联质谱法进行测量,游离睾酮(FT)由TT和SHBG来计算获得。以HGS<第10百分位数作为低HGS的临界值进行多变量回归分析。
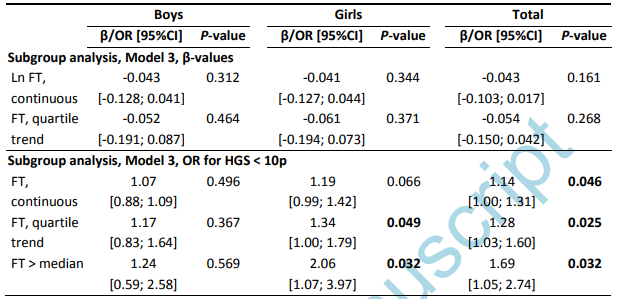
妊娠晚期FT浓度为0.004(0.002-0.007)nmol/L。男孩5岁时平均(SD)HGS为8.7(1.8)kg,女孩为8.1(1.7)kg,p<0.001。在调整母亲年龄、胎次、子代性别、5岁身高和体重后,较高的FT浓度与较低的HGS相关(β=-0.186,p=0.048)。FT>0.004nmol/L与5年HGS<第10百分位的较高风险相关,比值比[95%CI]为1.58[1.01;2.47],p=0.047(n=1,017);和1.69[1.05;2.74],在亚组分析中进一步调整儿童有组织的运动后,p=0.032(n=848)。在所有线性模型中都发现了较高FT浓度与子代较低的HGS相关,但并不总是具有统计学意义。子代HGS与孕妇TT和SHBG水平无关。
由此可见,妊娠晚期FT浓度与子女5岁时HGS评估的肌肉力量呈负相关,这可能表明母体FT对子代肌肉力量存在负面的影响。
原始出处:
Malene Dybdahl,et al.Maternal Testosterone Concentrations in Third Trimester and Offspring Handgrip Strength at 5 Years: Odense Child Cohort.JCEM.2022.https://academic.oup.com/jcem/advance-article/doi/10.1210/clinem/dgac143/6547253
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#JCE#
66
#握力#
75
#JCEM#
61
#孕晚期#
63
#浓度#
85