JAHA:全面!近40年来先天性心脏病的发病趋势分析
2021-07-19 MedSci原创 MedSci原创
单纯先天性心脏病患者的发病率和治疗率不断上升,而死亡率则不断下降,这表明人口在不断老化和增长。
先天性心脏病(CHD)是最常见的主要出生缺陷,占所有主要先天性缺陷的近三分之一。国际指南将CHD分为简单、中度和重度。由于过去几十年来诊断工具和治疗方法的改进,大多数患有CHD的儿童都能长大成人,而且据估计CHD在成人中的发病率已经超过了儿童。
以往的研究对单纯性 CHD 的预后趋势进行了调查,但都局限于单纯性 CHD 的亚组是基于超声心动图检查之前的旧队列,没有包括死亡风险的历年趋势,或者没有包括绝对风险,而是随时间变化的危险比,使得解释结果更加困难。
为了解决上述问题,来自丹麦哥本哈根大学心血管病专家开展了一项全国性的研究,研究了39年来由所有简单CHD组成的队列中,发病率、诊断年龄、死亡风险和侵入性手术概率的时间趋势。结果发表在JAHA杂志上。
研究人员利用全国范围内的丹麦登记册确定了1977年至2015年期间被诊断为孤立性室间隔缺损、房间隔缺损、动脉导管未闭或肺动脉狭窄的人。报告了每10万人年的发病率及95%的CI,1年有创心脏手术概率和诊断时的年龄按诊断年龄分层(儿童≤18岁,成人>18岁),以及1年全因死亡率按诊断年龄组分层(5-30岁,30-60岁,60岁以上)。
最终,该研究确定了15900名患有单纯先天性心脏病的人(室间隔缺损,35.2%;房间隔缺损,35.0%;动脉导管未闭,25.2%;肺动脉狭窄,4.6%),其中75.7%为儿童。从1977年到1986年和2007年到2015年,成人(8.8到31.8)和儿童房间隔缺损(26.6到150.8)的发病率均有所上升。
而室间隔缺损(72.1 [95% CI, 60.3-83.9] 到 115.4 [95% CI, 109.1-121.6])、动脉导管未闭(49.2 [95% CI, 39. 8-58.5]到102.2[95%CI,86.7-117.6])和肺动脉狭窄(5.7[95%CI,3.0-8.3]至21.5[95%CI,17.2-25.7])的发病率上升只有儿童中只观察到,成年人的发病率保持不变。
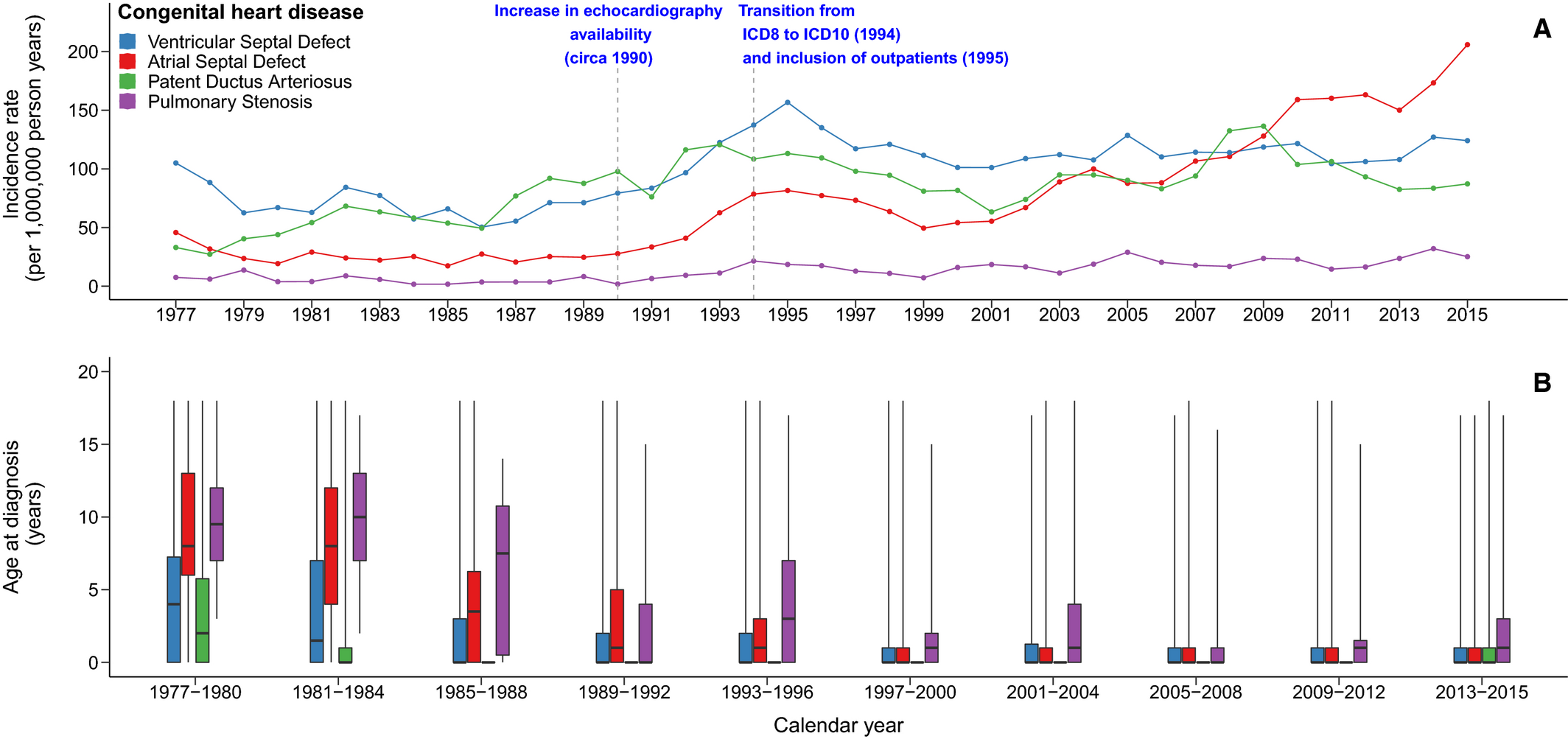
1977年至2015年期间,丹麦18岁前被诊断的人的发病率和诊断时的年龄。
从1977-1986年到2007-2015年,观察到所有年龄组的1年死亡率都有所下降(>60岁,30.1%-9.6%;30-60岁,9.5%-1.0%;5-30岁,1.9%-0.0%)。同时,儿童的1年手术概率下降(13.8%-6.6%),但成人的1年手术概率上升(13.3%-29.6%)。
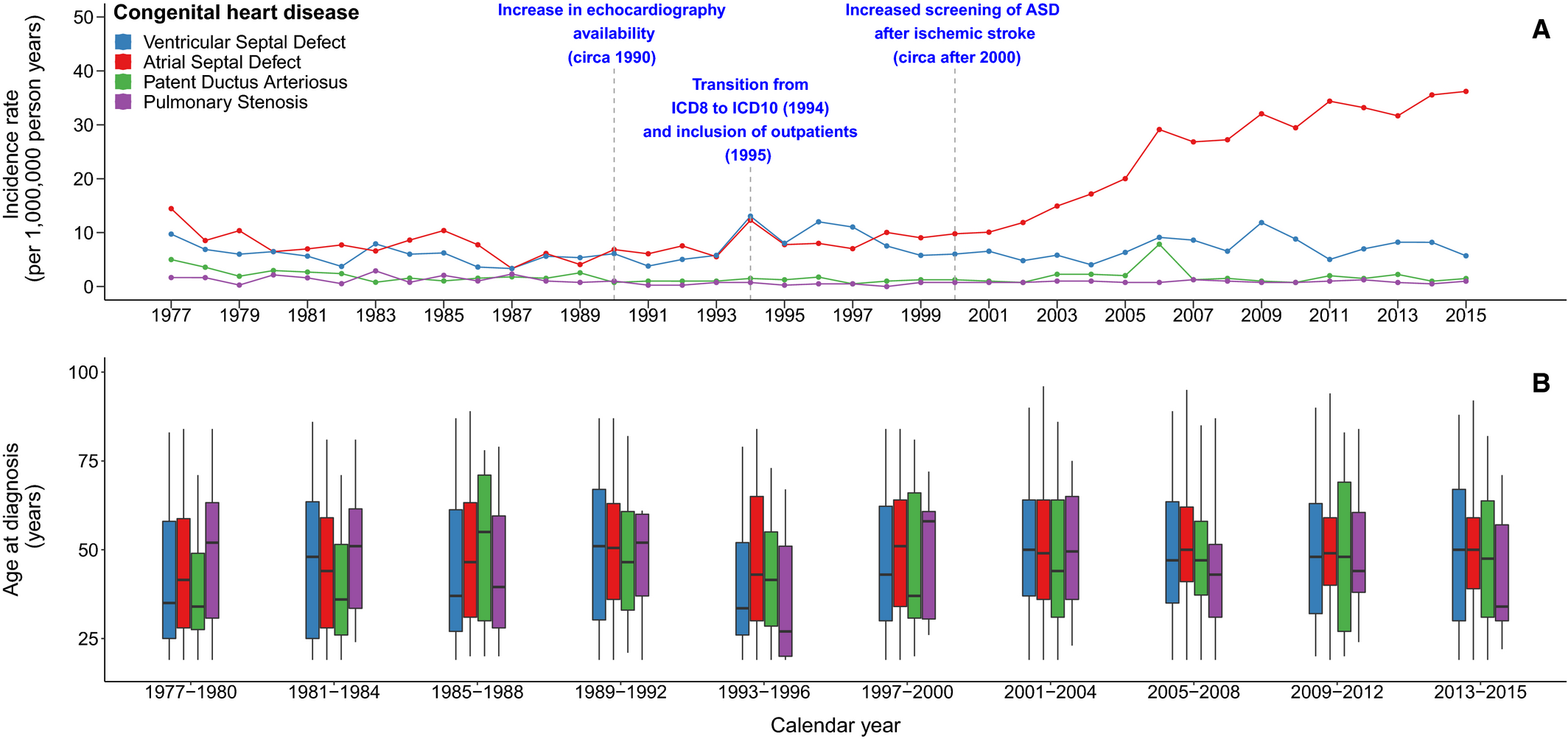
1977年至2015年期间,丹麦成人被诊断的人的发病率和诊断时的年龄。
研究人员指出,单纯先天性心脏病患者的发病率和治疗率不断上升,而死亡率则不断下降,这表明人口在不断老化和增长。需要对无症状的先天性心脏病采取更广泛的筛查方法,以启动及时的治疗和随访。
参考文献:
Time Trends in Simple Congenital Heart Disease Over 39 Years: A Danish Nationwide Study. https://doi.org/10.1161/JAHA.120.020375. Journal of the American Heart Association. ;0:e020375
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#趋势分析#
78
#发病趋势#
92
#AHA#
98
#先天性#
81
不错,很好
93