JNS:胸腰椎骨折PVP联合微创椎弓根内固定疗效良好
2013-08-26 JNS dxy
随着人均预期寿命的增加,骨质疏松性骨折的发病率越来越高,骨质疏松骨折患者典型的骨折部位主要包括髋关节周围及椎体。未行治疗的椎体骨质疏松骨折可造成严重的后果,严重者可至截瘫。 自1985年骨水泥应用于骨质疏松患者椎体骨折的治疗后,其应用已经日渐发展。目前PVP已经作为老龄人群骨质疏松性椎体骨折的一个标准治疗术式,多项前瞻性随机对照研究表明PVP术后患者疼痛改善,功能恢复等较传统开放手术均有
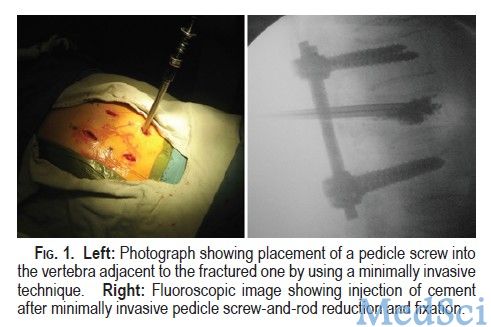
图1:左,微创化技术将椎弓根螺钉置入骨折椎体的邻近节段;右图,椎弓根螺钉置入完成后钉棒加压,骨折复位后进行PVP。
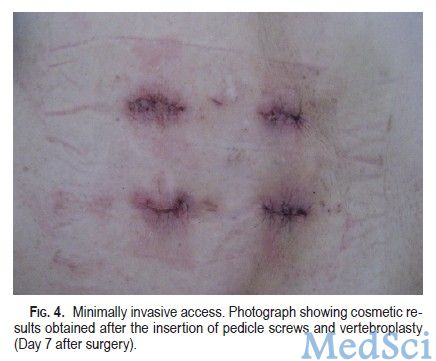
图4:微创手术入路。照片显示椎弓根螺钉置入+PVP后具有较好的外观形态
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#腰椎骨#
58
#PVP#
113
#胸腰椎骨折#
62
#腰椎#
66
#微创#
65
#内固定#
82