Cell:三阴性乳腺癌细胞可唆使正常细胞模仿病毒帮助肿瘤扩散并耐药
2017-07-21 佚名 肿瘤医学论坛
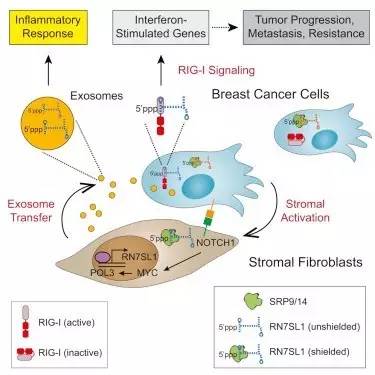
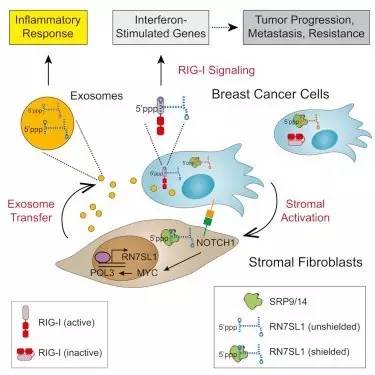
2017年7月13日,美国爱思唯尔旗下《细胞》正式发表宾夕法尼亚大学、罗格斯大学的研究报告稿,发现为何某些乳腺癌比其他乳腺癌更有浸润性、癌细胞如何诱骗正常细胞像病毒一样释放特殊的RNA帮助肿瘤生长、耐药、转移。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#CEL#
83
#阴性乳腺癌#
62
#Cell#
92
学习一下谢谢分享
89
学习一下谢谢分享
102
学习一下谢谢分享
111
学习一下谢谢分享
111
学习一下谢谢分享
112
学习一下谢谢分享
78
乳腺癌转移机制是现在的研究热点,高水平文章总能带给我们全新的视角
54