JAMA Oncol:三个2带一个王:三药联合贝伐珠单抗,肠癌肝转移手术可以行
2017-07-18 王东亮 肿瘤资讯
概述 结直肠癌是世界上致死率最高的肿瘤之一,大约25%的患者首次诊断时即同时合并肝脏转移,另有50%的患者在后续的治疗过程中或早或晚会出现肝脏转移。在诸多治疗手段中,只有手术切除才可以提供根治的可能,接受了肝脏转移灶切除的患者五年生存率可达到50%,但大多数肝转移患者都由于病灶过于广泛而无法接受手术治疗。随着化疗、靶向治疗的有效性提高及外科手术技术的进步,有一些既往认定为不可切除的肝转移患者
概述
结直肠癌是世界上致死率最高的肿瘤之一,大约25%的患者首次诊断时即同时合并肝脏转移,另有50%的患者在后续的治疗过程中或早或晚会出现肝脏转移。在诸多治疗手段中,只有手术切除才可以提供根治的可能,接受了肝脏转移灶切除的患者五年生存率可达到50%,但大多数肝转移患者都由于病灶过于广泛而无法接受手术治疗。随着化疗、靶向治疗的有效性提高及外科手术技术的进步,有一些既往认定为不可切除的肝转移患者经过转化治疗后也可以转变成可手术的患者,而接受转化治疗成功获得手术的患者,其生存期与那些首次诊断即为可切除的患者类似。研究者发现转化治疗的有效率与肝脏转移灶切除率之间存在着密切的关联,而靶向药物可以显着提升客观缓解率进而提升患者接受手术切除的概率。在诸多转化治疗方案中,有研究报道由氟尿嘧啶、奥沙利铂、伊立替康及贝伐珠单抗组成的FOLFOXIRI-Bev方案治疗仅限于肝脏转移的客观有效率可高达80%,约32-40%的患者可以接受根治性切除。本文就FOLFOXIRI-Bev方案治疗仅肝脏转移且初始不可切除的结直肠癌患者的有效性、转化手术率及长期生存等进行系统性回顾及汇总分析。
方法
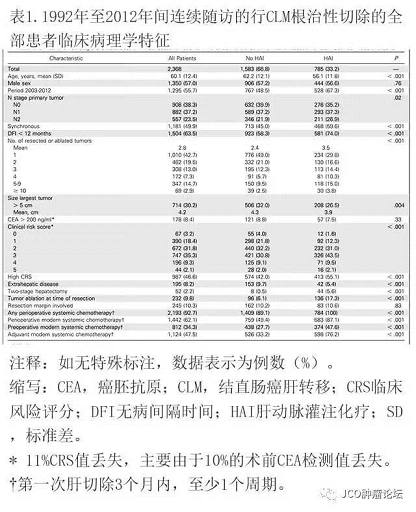
文献回顾采用PRISMA指南标准,以FOLFOXIRI/bevacizumab/colorectal cancer为检索词从各大数据库中进行检索,研究发表时间截止在2016年10月。本研究主要研究终点为总切除率、次要研究终点为R0切除率、客观缓解率、中位无进展生存期及总生存期。
结果
本研究总计纳入了自2010年至2016年的1项前瞻性队列研究,2项回顾性队列研究,2项Ⅱ期研究,1项Ⅰ-Ⅱ其研究,4项Ⅱ期随机研究,1项Ⅲ期随机研究。在8项研究中,经统计后汇总总切除率为39.1%(95%CI, 26.9%-52.8%),汇总R0切除率为28.1%(95%CI, 18.1%-40.8%),汇总客观有效率为69%(95%CI, 68%-72%),汇总中位生存期为30.2个月,无进展生存期为12.4个月。
讨论
近年间由于靶向药物的面世,联合化疗可以一定程度上扩大手术的适应症,转移性结直肠癌的治疗近年间处于快速进步阶段,患者的生存期得到了显着延长。而患者只有接受了根治性切除,生存期才可以获得显着获益。所以研究者们为了追求提升根治性切除的几率而在转化治疗中进行了一系列探索。本研究确定了高强度化疗联合贝伐珠单抗可以有效缩瘤、提升手术切除的概率——FOLFOXIRI-Bev方案可以为患者带来70%的客观缓解率,40%的初始不可切除结直肠癌肝转移患者有机会可以接受手术切除,25%的患者可以接受根治性切除。在临床实践当中,当遇到结直肠癌肝转移患者时,应首先经多学科讨论环节认定患者初始是否能够接受手术,而这样的原因在于近年间对于手术可切除的标准在不断的扩展,越来越多的患者可以在化疗及靶向治疗的支持下转化成为可手术的类型。转化治疗的具体方案可由氟尿嘧啶、伊立替康、奥沙利铂等化学药物组成,也可联合抗血管生成药物,如贝伐珠单抗,或联合表皮生长因子单抗,例如西妥昔单抗等。针对仅有肝脏转移的转移性结直肠癌患者来说,转化治疗的目的就是为了肝脏肿瘤变为可切除,所以客观有效率为首要的追求目标。近期有Meta分析表明,在化疗的基础上,靶向药物的加入可以显着提高肝脏病灶潜在可切除的转移性结直肠癌患者的手术概率。并且本研究数据要优于既往研究报道的两药方案联合西妥昔单抗R0切除率(11.8-38%)。尽管本研究最终汇总的中位总生存及无进展生存结果并不惊艳,但与既往的TRIBE 这一Ⅲ期临床研究结果保持一致,说明即便是初始不可切除的转移性结直肠癌患者,这一预后不良的群体仍可以通过有效的治疗进而接受手术而获得更好的生存时间。本研究结果证明三药方案联合贝伐珠单抗可以为患者带来更好的客观缓解率,这样不仅可以控制疾病的进展,还可以快速地缩小肿瘤体积,进而为后续的手术争取可能性。在临床实践过程中,转移性结直肠癌患者应接受多学科会诊讨论后,方可将化疗、靶向治疗及手术等治疗手段的优势优化到最佳状态,才可以获得更长的生存期。
专业点评:由于转移性结直肠癌的肝转移发生几率很大,很大程度上影响了患者的生存期,并且仍然仅有手术才可以为患者带来根治性的治疗,改善生存期。但结直肠癌肝脏转移灶对于化疗、靶向治疗的响应程度仍然处于“少女心”阶段——完全不响应的概率并不大,但响应到能达到目标(可手术)的概率也不大,所以近年间这部分患者的主要焦点就在于如何能向前勇敢的迈出这一步——提升肝转移灶转化治疗的响应程度。结直肠癌的化疗及靶向药物仅有可数的几种,无论如何优化组合,都会遇到天花板效应,疗效无法继续提升。所以,可选的解决方案就是这样“三个2带一个王”的办法,尽管在既往一些研究中可以观察到一定的疗效提升、手术转化率优化的趋势,但尚缺乏汇总分析。本研究综合了既往发表的相关研究,从更高级别循证医学证据角度证实了三药联合贝伐珠单抗的方案可以更加有效的缩瘤,并转化成可手术案例。具体到国内情况,这种方案从理论上是可以应用了,但从理念上还需转变。传统来说,一般认为国人的体质差于西方,耐受程度较弱,所以类似这样的强力方案,国内医生在顺铂与表阿霉素都要分开天数使用的情况下,肯定是要心存疑虑的。这样的三药方案其实在国内一些中心早有应用,通过合理的优化药物剂量,国人也是可以良好耐受的。并已有国内中心在设计三药方案用于局部进展期直肠癌的术前治疗的相关临床研究,说明此方案的可适用程度要比想象中好很多。所以就好比易筋经已经公开于天下了,但具体到某一个体能不能练成,就要看各自的努力及其他因素了。
原始出处:
Gianluca Tomasello, Fausto Petrelli, et al. FOLFOXIRI Plus Bevacizumab as Conversion Therapy for Patients With Initially Unresectable Metastatic Colorectal Cancer A Systematic Review and Pooled Analysis. JAMA Oncol. 2017;3(7):e170278. doi:10.1001/jamaoncol.2017.0278
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Oncol#
40
#贝伐珠#
38
#肝转移#
45
#贝伐#
42
学习了学习了学习了学习了
52