Stroke:急性大动脉闭塞性卒中,患者进城,还是医生下乡?
2018-01-09 杨中华 脑血管病及重症文献导读
血管内治疗是急性缺血性卒中治疗的有效方法,但是受到时间窗的限制。在缺血的情况下神经组织迅速死亡,因此缩短治疗时间是卒中治疗的主要目标。
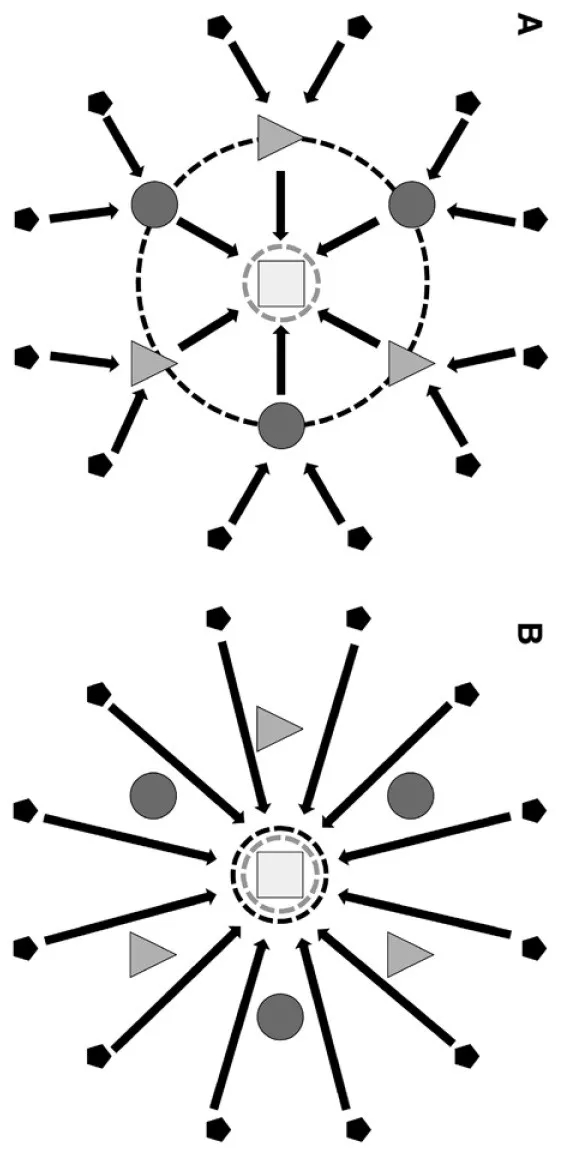
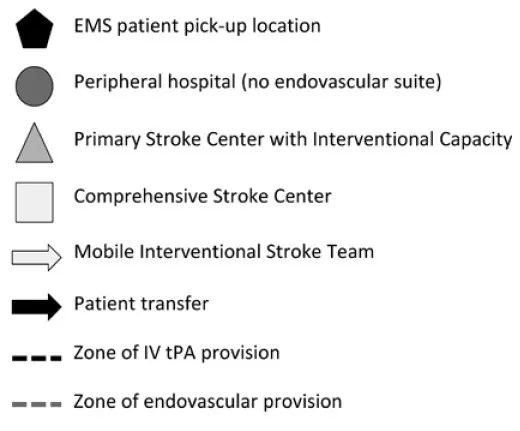
在2015年以前,静脉溶栓是治疗急性缺血性卒中唯一的手段。对于需要静脉rtPA溶栓的患者,两组最常用的转运模式为drip-and-ship(A图)以及mothership。drip-and-ship(B图)模式是将患者转运到最近的医院,把发病到静脉溶栓的时间降到最低。mothership模式是将患者直接转运到高级卒中中心,把发病到高级治疗(包括血管内治疗)的时间降到最低。
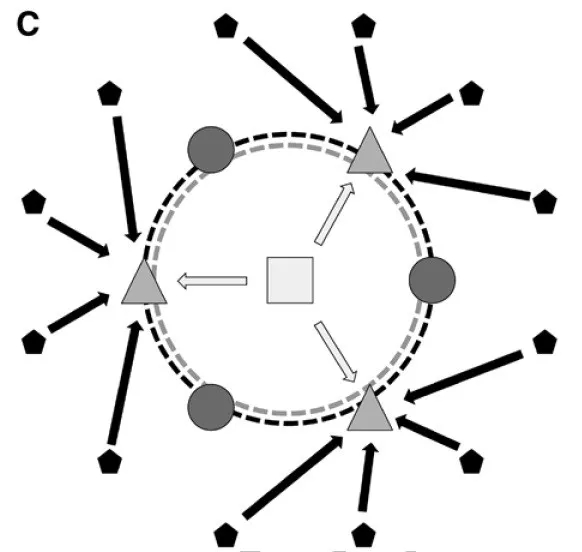
trip-and-treat模式(C图)是指高级卒中中心的移动介入团队直接到初级卒中中心救治需要血管内治疗的患者。移动介入卒中团队(mobile interventional stroke team,MIST)包括受过血管内治疗训练的主治医师,进修医生(fellow),放射技术人员。急救系统把患者送到初级卒中中心,一旦诊断大动脉闭塞性急性缺血性卒中,立即通知MIST。MIST立即到卫星医院提供血管内治疗。
2017年12月来自纽约的Daniel Wei等在Stroke上发表了他们的研究结果,目的在于比较trip-and-treat模式和传统drip-and-ship模式的优劣。
该研究回顾性分析了86例接受了血管内治疗的连续大动脉闭塞性急性缺血性卒中患者。这些患者分为两个队列:trip-and-treat组39例,drip-and-ship组47例。主要终点为门-穿刺时间,定义为患者到达医院和动脉穿刺之间的时间。
他们发现trip-and-treat组门-穿刺时间为143分钟,drip-and-ship组为222分钟(P = 0.0887);门-再通时间分别为199分钟和267分钟(P < 0.0001);对于入院到出院NIHSS评分的改善,trip-and-treat有获益的趋势(P = 0.0704)。
最终作者认为与drip-and-ship模式相比,trip-and-treat模式能够缩短血管内治疗的时间。
原始出处:
Wei D,et al.Mobile Interventional Stroke Teams Lead to Faster Treatment Times for Thrombectomy in Large Vessel Occlusion.Stroke. 2017 Dec;48(12):3295-3300. doi: 10.1161/STROKEAHA.117.018149. Epub 2017 Nov 16.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#动脉闭塞#
56
#大动脉闭塞#
79
#闭塞性卒中#
77
^_^^_^^_^^_^^_^
93
学习了.涨知识
97