JACC:这一不起眼的坏“血脂”,中风风险增加6成,还跟动脉粥样硬化进展有关!
2022-01-25 MedSci原创 MedSci原创
脂蛋白(a)(Lp[a])已被广泛认为是一个普遍的和独立的心血管危险因素。
脂蛋白(a)(Lp[a])已被广泛认为是一个普遍的和独立的心血管危险因素。最近的临床试验的事后分析证实,Lpa是残留心血管风险的有效标志物,即使在接受强化降脂治疗的患者中也是如此。
目前的指南建议测量Lp(a)来识别终生有高风险的动脉粥样硬化性心血管疾病(ASCVD)患者。尽管专门用于降低LPa的疗法的结果研究正在进行,但由LPa介导的ASCVD风险增加的确切机制仍有争议。
不久前发表在JACC杂志上的研究显示,与LP(a)水平< 10 mg/dl (<18 nmol/l:第1至第50百分位)的个体相比,对于LP(a)> 93mg/dl (>199 nmol/L:第96至第100百分位)的个体,缺血性卒中的风险增加60%(OR=1.60,95%CI: 1.24-2.05)。
为了进一步探讨Lpa是否与不良动脉粥样硬化斑块进展有关,来自荷兰阿姆斯特丹大学心血管科学学院血管医学系的专家开展了相关研究,结果发表在JACC杂志上。
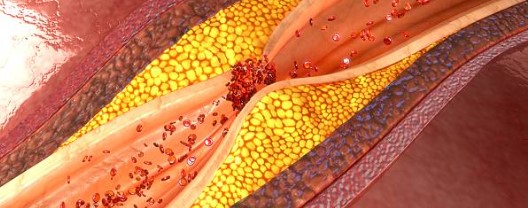
研究人员对接受冠状动脉CTA检查的晚期稳定冠状动脉疾病患者在基线和12个月时测量Lp(a),以评估总斑块、钙化斑块、非钙化斑块和低衰减斑块(坏死核心)的进展情况。高LPa被定义为Lpa≥70mg/dL。在调整体重指数BMI、节段参与评分和ASSIGN评分后,使用线性回归分析评估Lp(a)与斑块进展的关系。
结果共有191名患者(65.9±8.3岁;152名[80%]男性)被纳入分析,高Lpa组和低Lpa组的中值分别为100(范围:82-115)mg/dL和10(范围:5-24)mg/dL。在基线时,两组患者ASCVD的严重程度或斑块负担没有差异。

与低Lpa组患者相比,高Lpa组患者的低回声斑块进展速度更快(26.2 ± 88.4 mm3 vs -0.7 ± 50.1 mm3;P = 0.020)。多变量线性回归分析证实了Lp(a)和低回声斑块体积进展之间的关系(β = 每50 mg/dL Lp(a)增加10.5%,95% CI: 0.7%-20.3%)。在总的、钙化的和非钙化的斑块体积进展方面没有差异。
综上,在晚期稳定型ASCVD患者中,Lp(a)与冠状动脉斑块坏死核心的加速进展有关。这可能解释了Lp(a)与心肌梗死的高残留风险之间的关联,为Lp(a)作为动脉粥样硬化的治疗目标提供了支持。
参考文献:
Association of Lipoprotein(a) With Atherosclerotic Plaque Progression. J Am Coll Cardiol. 2022 Jan, 79 (3) 223–233
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#中风风险#
108
#粥样硬化#
85
#JACC#
109
LP(a)有无治疗方法
86
应该重视
88
#ACC#
88
学习了
96
学习
84
学习学习
102
学习#学习#
69