NEJM:甲状腺相关性并发症-案例报道
2016-07-21 chenshuo 译 MedSci原创
男性患者,56岁,近日因甲状腺相关性皮肤问题到院就诊。据该患者称,在3年前他曾被诊断患有甲状腺相关眼病和皮肤病。当时接受了放射性碘消融术进行治疗。
男性患者,56岁,近日因甲状腺相关性皮肤问题到院就诊。
据该患者称,在3年前他曾被诊断患有甲状腺相关眼病和皮肤病。当时接受了放射性碘消融术进行治疗。
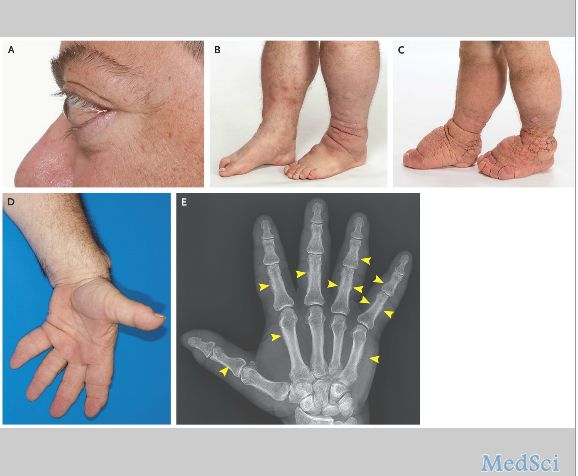
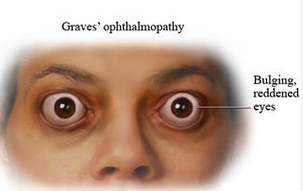
经治疗1年后,其开始出现眼球突出和胫前粘液性水肿症状(如图A和B所示)。之后该患者又接受了眼眶减压术。
在这次就诊中,体格检查发现其小腿部和脚部的皮肤病变越发严重,类似于橡皮肿样(如图C)。此外,其双手相对于以前显得更加的粗大,双手手指像棍棒形(如图D)。
手掌部X光拍片检查显示多指骨和掌骨骨膜炎(如图E,箭头),另外还有软组织弥漫性肿胀,与甲状腺毒症的变化一致,这与Graves病的罕见表现类似。
实验室检查结果表明,促甲状腺素受体抗体水平>40 IU/L(正常范围,≤1.75 IU/L)。
最后,该患者接受静脉注射免疫球蛋白和利妥昔单抗药物联合治疗。在接下来的几个月随访中,发现该患者的症状得到了很好地控制。
原始出处:
Carlo Guerrero, M.D.Mark R. Pittelkow, M.D.Thyroid Ophthalmopathy, Dermopathy, and AcropachyN Engl J Med .July 21, 2016本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#相关性#
57
#并发#
66
文章很好,继续关注
84
文章很好,非常有益
102
不错哦,会学到很多
79
学习新知识了,感谢分享
84
很好,不错,以后会多学习
89