血脂水平与多系统萎缩患病风险的相关性
2016-09-28 张书语 田杰等 《中华神经科杂志》
多系统萎缩(multiple system atrophy,MSA)是一组成年期发病的进行性神经系统退行性疾病,临床表现为不同程度的自主神经功能障碍、对左旋多巴类药物反应不良的帕金森样症状、小脑性共济失调和锥体束征等症状[1]。主要病理表现为α-突触核蛋白在少突胶质细胞中的堆积[2]。根据症状可将MSA分为帕金森病样症状为主型(MSA-P)、小脑症状为主型(MSΑ-C)及自主神经功能障碍为主型
多系统萎缩(multiple system atrophy,MSA)是一组成年期发病的进行性神经系统退行性疾病,临床表现为不同程度的自主神经功能障碍、对左旋多巴类药物反应不良的帕金森样症状、小脑性共济失调和锥体束征等症状[1]。主要病理表现为α-突触核蛋白在少突胶质细胞中的堆积[2]。根据症状可将MSA分为帕金森病样症状为主型(MSA-P)、小脑症状为主型(MSΑ-C)及自主神经功能障碍为主型(MSΑ-A)3个亚型[3]。目前该病病因不明,且早期临床表现与帕金森病、脊髓小脑共济失调等疾病有重叠现象[4],易被误诊,因此提供更多的诊断依据尤为重要。既往研究提示血脂水平可能与MSA患病相关[5,6],但MSA各亚型与血脂之间关系尚不明确。我们通过比较MSA患者与健康对照及MSA各亚型患者与健康对照间的血脂水平差异,尝试探索MSA早期的生物学标志物。 一、研究对象 连续纳入2011年1月至2015年3月在郑州大学第一附属医院就诊的MSA患者,均符合Gilman等[7]提出的诊断标准;连续纳入同时期内该院就诊的年龄、性别相匹配的无神经系统疾病的健康对照,所有研究对象均未服用降脂药物,无甲状腺功能障碍,无严重肝肾功能疾病,无脑卒中、癫痫等神经系统疾病,且均为本地区居民,饮食结构及生活习惯相似。本研究经过郑州大学第一附属医院伦理委员会批准,所有研究对象包括健康对照均签署书面的知情同意书。 二、方法 所有受试者空腹12 h后,采用全自动生化分析仪(Olympus AU 5400型)检测血清总胆固醇、甘油三酯、低密度脂蛋白胆固醇、高密度脂蛋白胆固醇的水平;由经统一培训的神经内科医生详细收集所有受试者年龄、性别、吸烟史、饮酒史、既往史,记录所有患者发病年龄、疾病病程、吞咽情况,并进行Hoehn-Yahr(H-Y)分期。 三、统计学分析 采用SPSS16.0版进行统计学处理,正态分布的计量资料用均数±标准差表示,计数资料用例(%)表示。采取两独立样本均数t检验比较患者与健康对照血脂各指标水平差异;采用LSD-t检验法比较MSA各亚型之间及各亚型与对照组之间血脂水平差异;根据病例组血脂水平将血脂行四分位数分层,以低四分位数组为参考,采用多元Logistic 回归法分别比较不同水平总胆固醇、甘油三酯、高密度脂蛋白及低密度脂蛋白组MSA患病倾向;采用Spearman相关法分析MSA患者总胆固醇、甘油三酯、高密度脂蛋白胆固醇、低密度脂蛋白胆固醇水平与发病年龄、疾病病程及H-Y分期的相关性。P< 0.05为差异有统计学意义。 一、病例组与对照组基线资料 共纳入MSA病例组195例,平均年龄(58.18±8.29)岁,男性98例,女性97例;连续纳入同时期内该院就诊的年龄、性别匹配的无神经系统疾病的健康对照195名,平均年龄(56.98±10.23)岁,男性96名,女性99名。病例组总胆固醇、甘油三酯及低密度脂蛋白胆固醇水平均较对照组降低,差异有统计学意义(表1)。 根据性别分组后,男性患者高密度脂蛋白胆固醇水平较对照组降低,差异有统计学意义,总胆固醇、甘油三酯及低密度脂蛋白胆固醇水平均低于对照组,但差异无统计学意义;在女性中,病例组甘油三酯水平较对照组降低,差异有统计学意义,总胆固醇、高密度脂蛋白胆固醇及低密度脂蛋白胆固醇水平均低于对照组,但差异无统计学意义(表2)。 MSA 各亚型患者年龄与对照组比较差异无统计学意义。MSA-P型患者总胆固醇、甘油三酯水平低于对照组,差异有统计学意义,MSA-C及MSA-A型患者总胆固醇、甘油三酯水平与对照组比较及各亚型患者高密度脂蛋白胆固醇及低密度脂蛋白胆固醇水平与对照组比较差异均无统计学意义,MSA各亚型之间血脂各指标比较差异无统计学意义(表3)。 根据病例组血脂各指标水平进行四分位数分层,在校正年龄、性别、吸烟史、饮酒史、高血压病史及糖尿病病史后采用多元Logistic回归分析(表4)发现,高水平甘油三酯、高密度脂蛋白胆固醇组与低水平组比较,OR值分别为0.31(95% CI 0.15~0.65, P=0.002)及0.38(95% CI0.17~0.83,P=0.016),在男性人群中,这两项比较的OR=0.26, 95% CI 0.09~0.80,P=0.018及OR=0.20, 95% CI 0.06~0.70, P=0.011;在女性人群中,高水平甘油三酯组与低水平组比较,OR=0.32(95% CI 0.11~0.99,P=0.047)。 Spearman相关分析显示,MSA患者高密度脂蛋白与发病年龄呈正相关(r= 0.15,P<0.05),其余血脂指标与发病年龄相关性无统计学意义;血脂水平与疾病病程、H-Y分期间相关性无统计学意义。 目前认为MSA的主要病理改变为α-突触核蛋白在少突胶质细胞的异常聚集[8],因此与帕金森病、路易体痴呆等疾病同属于α-突触核蛋白病。研究表明α-突触核蛋白基因多态性与MSA病理改变相关,α-突触核蛋白在脂质运输及生物膜合成中发挥作用,脑内异常的胆固醇代谢可影响α-突触核蛋白的聚集[9]。而大脑是富含胆固醇的器官,胆固醇失稳态会影响神经元及突触的结构、功能。同时胆固醇是体内抗氧化剂辅酶Q10代谢的重要辅助因子,总胆固醇水平降低,可降低辅酶Q10水平[10]。总胆固醇、甘油三酯及低密度脂蛋白胆固醇水平增高及高密度脂蛋白胆固醇水平降低是卒中的危险因素,而临床上发现帕金森病、MSA患者卒中风险降低。综上,我们考虑血脂代谢异常可能与MSA发病相关。 血脂是血浆中甘油三酯、胆固醇、类脂的总称。胆固醇是细胞膜的重要组成部分,在脑组织中参与神经轴突的信号传递,神经的生长及修复,突触的产生[11]。我们发现MSA患者总胆固醇水平低于健康对照,原因可能是胆固醇和辅酶Q10有相同的生物合成途径,胆固醇可调节血清辅酶Q10浓度[12,13]。研究表明辅酶Q10是线粒体电子传递链中的辅助因子,可抑制氧化应激、阻止线粒体调控的细胞凋亡等[14],辅酶Q10减少可导致线粒体功能障碍[15],导致多巴胺能神经元变性死亡;同时辅酶Q10是一种内源性抗氧化剂,辅酶Q10浓度降低使机体倾向于氧化应激状态,导致多巴胺能神经元变性及丢失。辅酶Q10参与清除自由基、减少氧化应激反应、调节线粒体功能障碍及稳定细胞膜等过程,可改善早期PD患者症状[16]。既往研究表明降脂药物降低胆固醇水平后可改善α-突触核蛋白的异常增多[17],且动物实验表明降低胆固醇水平可减少α-突触核蛋白在神经元的聚集,使帕金森病患者获益[18]。综上,胆固醇浓度低可导致辅酶Q10浓度降低,直接或间接导致氧化应激障碍,引起神经元变性死亡,增加MSA患病风险。 一项关于帕金森病的病例对照研究发现低密度脂蛋白胆固醇水平降低与帕金森病患病风险增加相关[17]。载脂蛋白E(ApoE)参与介导脂类的转运和代谢。ApoE基因被认为是阿尔茨海默病的遗传风险[19],且与帕金森病患病相关[20]。而本研究结果提示低密度脂蛋白胆固醇可能与MSA发病相关。载脂蛋白A1(ApoA1)是高密度脂蛋白胆固醇的主要成分[21],在一项利用123Iβ-CIT SPECT多巴胺转运体(DAT)显像技术的研究中发现,血浆ApoA1水平与DAT再摄取程度相关,ApoA1水平越低,DAT缺乏越严重[22]。研究表明血清ApoA1水平降低可减弱对氧磷酶活性,而对氧磷酶可使低密度脂蛋白胆固醇向27-羟胆固醇转化能力降低,增加α-突触核蛋白水平并引起细胞凋亡[23]。因此可推测,高密度脂蛋白胆固醇水平降低可增加MSA等疾病发生风险,但具体致病机制仍需要进一步研究证实。 综上,我们通过分析血脂水平与多系统萎缩患者之间的关系,认为甘油三酯、高密度脂蛋白胆固醇水平降低可能与MSA患病相关,且高密度脂蛋白胆固醇水平越低,MSA发病年龄可能越小,但需要前瞻性队列研究证实。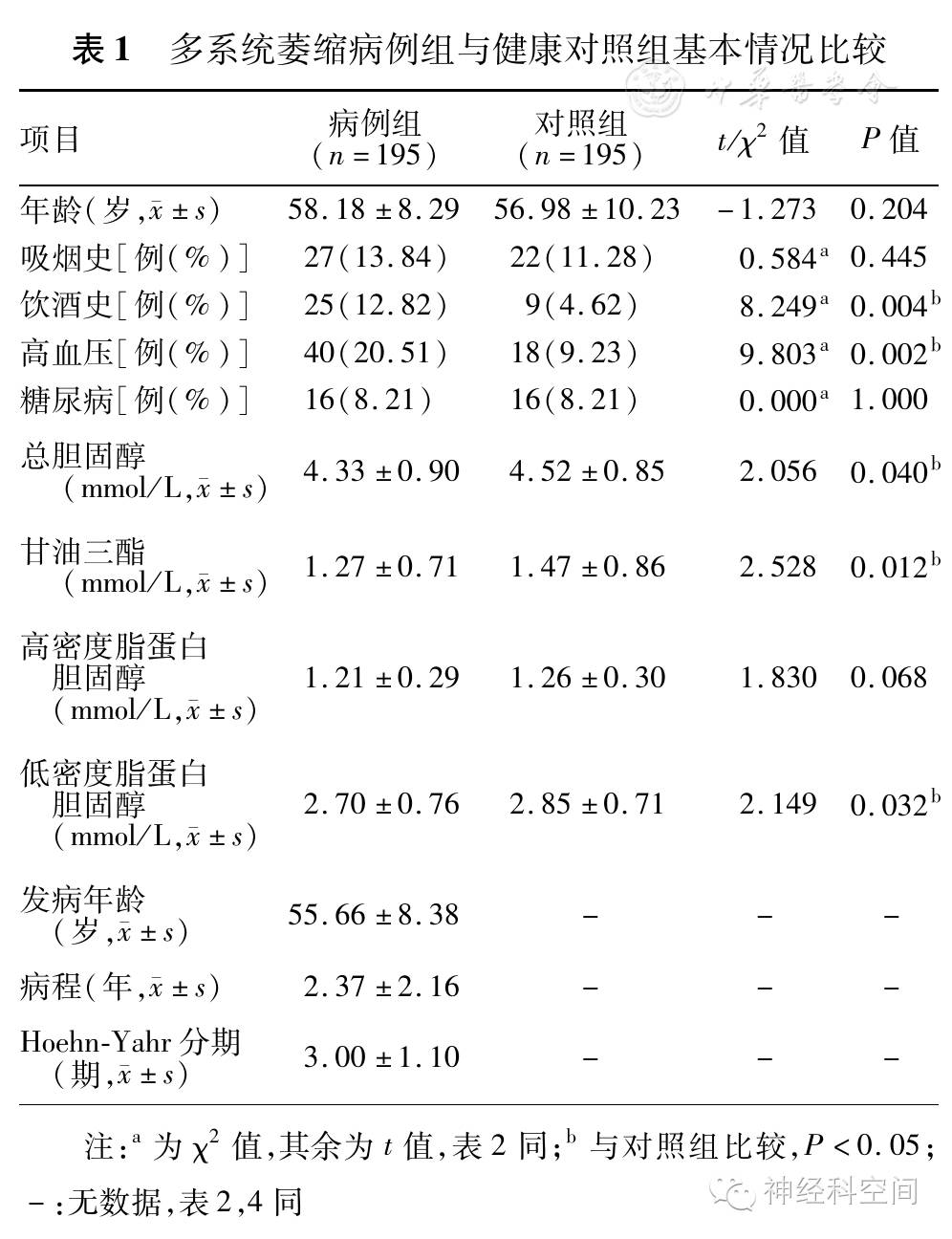
表1 多系统萎缩病例组与健康对照组基本情况比较
表2 MSA病例组与健康对照组根据性别分组后比较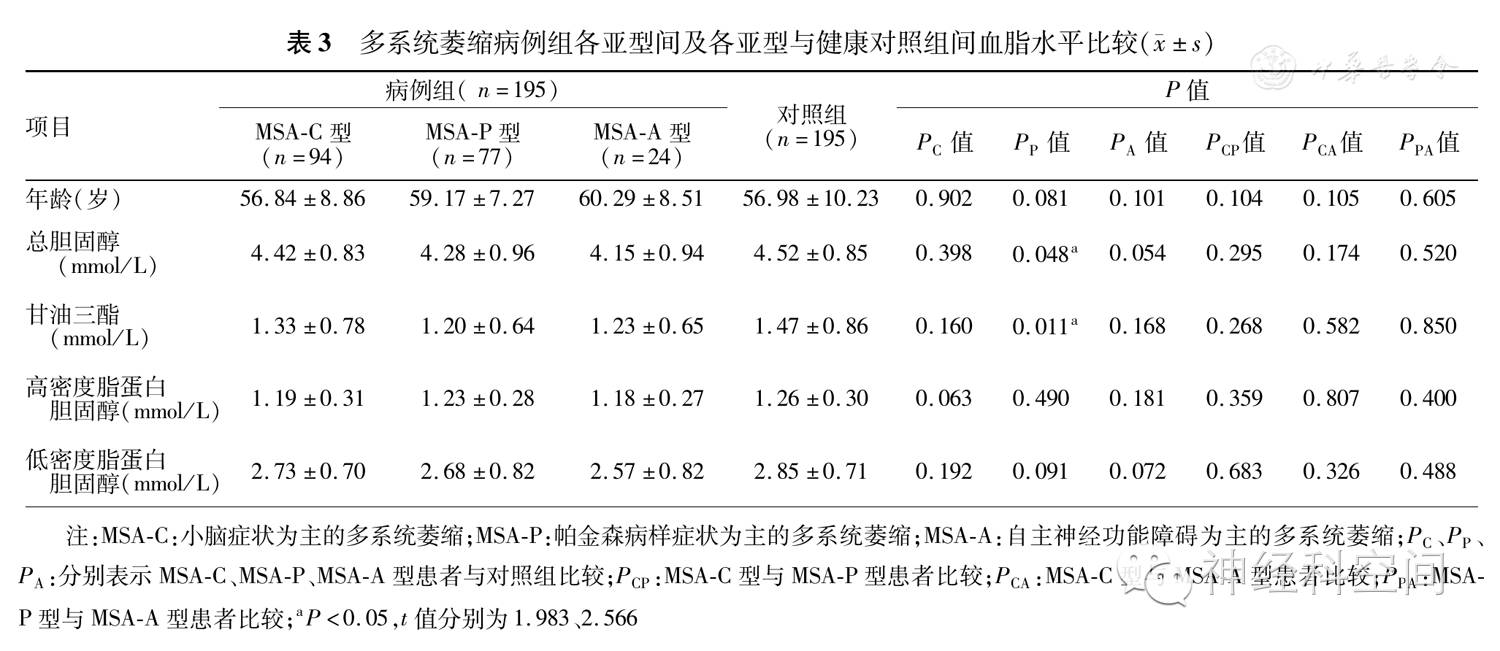
表3 多系统萎缩病例组各亚型间及各亚型与健康对照组间血脂水平比较( ±s)
±s)FDA/0.jpg" src="https://img.medsci.cn/webeditor/uploadfile/201609/20160928210657717.jpg&tp=webp&wxfrom=5&wx_lazy=1" data-fail="0" style="margin: 0px; padding: 0px; height: auto !important; max-width: 100%; box-sizing: border-box !important; word-wrap: break-word !important; width: auto !important; visibility: visible !important;">
表4 根据血脂各指标水平分层后的多元Logistic回归分析结果
参考文献略
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#血脂水#
83
#相关性#
90
#萎缩#
81
#血脂水平#
104
学习并分享
81
#患病风险#
71
#多系统萎缩#
81