Eur Radiol:软组织肉瘤患者要警惕胸部转移的存在!
2021-02-23 shaosai MedSci原创
肺是软组织肉瘤转移最常见的部位,由于对肺转移性病灶进行手术切除可改善患者预后,因此,在最初诊断软组组肉瘤时应进行胸部CT扫描以明确肺转移病灶是否存在。
软组织肉瘤(Soft tissue sarcoms, STS)是指间叶起源的恶性病变,有多种组织学亚型,目前根据世界卫生组织软组织和骨肿瘤分类2020进行分类。它们约占成人恶性肿瘤的1%。肺是STS转移最常见的部位,由于对肺转移性病灶进行手术切除可改善患者预后,因此,在最初诊断STS时应进行胸部CT扫描以明确肺转移病灶是否存在。
据报道,6-13%的STS病例中发生局部复发(LR),重要的危险因素包括肿瘤组织学级别较高以及多灶性阳性切缘。LR的发生常提示预后较差。临床上怀疑LR时应行磁共振成像(MRI)检查,并行穿刺活检进行确认。目前英国的指南规定在确诊LR时应重复胸部CT检查,但现阶段仍未有任何数据支持这一声明。
近日,发表在European Radiology杂志的一项研究探讨了躯干和四肢STS首次LR时胸部CT再分期的价值,为临床治疗方案的选择提供了新的依据。
回顾性的分析了2007年5月至2018年4月间所有诊断为复发性STS的患者。收集的数据包括患者年龄和性别、原发STS的部位、达LR的时间、复发部位、原发肿瘤分级、复发肿瘤分级、最初胸部CT分期特点、以及胸部CT再分期肺转移的发病率。
本研究共纳入109例患者(男性68例,女性41例,平均年龄56岁,范围9-92岁)。最常见的肿瘤亚型为粘液纤维肉瘤(27.5%)、未分化的多形性/梭形细胞肉瘤(20.2%)、滑膜肉瘤(10.1%)和恶性周围神经鞘瘤(10.1%)。最初胸部CT分期检查显示77例患者中有1例(1.3%)有肺转移。平均达LR时间为30.8个月(3 ~ 224个月)。109例患者中26例(23.9%)经胸部CT再分期诊断为肺转移,最常见的是3级STS(36.1%)。多形性肉瘤(85.7%)和未分化梭形细胞肉瘤(33.3%)是首次LR时两种最常见的伴有肺转移的肿瘤亚型。
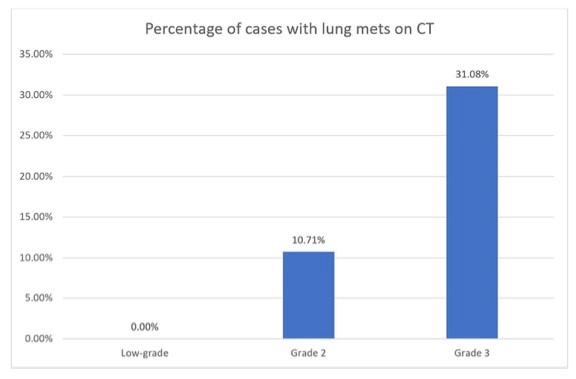
图1原发性STS的组织学分级与再分期CT上肺转移发生率的比较。结果表明,原发肿瘤分级越高,肺转移发生率越高
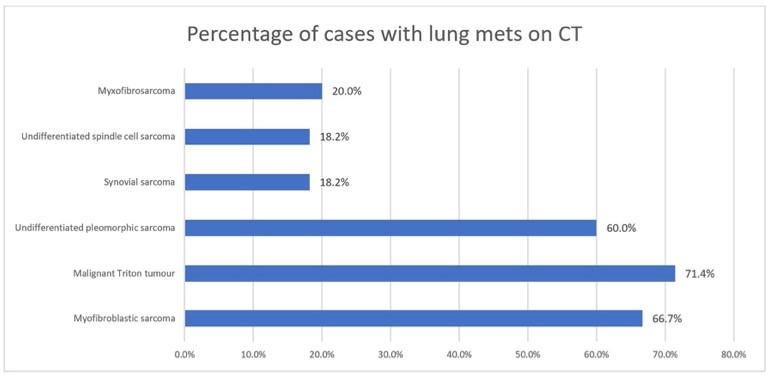
图2 STS的组织学亚型与再分期CT肺转移的发生率。结果表明,多形性肉瘤(85.7%)和未分化梭形细胞肉瘤(33.3%)是首次LR时两种最常见的伴有肺转移的肿瘤亚型。
目前的研究表明躯干或四肢STS的LR患者肺转移的发生率非常高,这支持英国指南所提出的在首次LR时应进行重复胸部CT 检查的要求,提示了临床在STS患者发生局部复发时应警惕肺转移的可能性,这为治疗方案的选择提供了新的依据。
原始出处:
Mirza S Baig,Wais Habib,Veronica Attard,et al. The value of re-staging chest CT at first local recurrence of extremity and trunk soft tissue sarcoma. DOI:10.1007/s00330-020-07366-8
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
.jpg)









学习了
89
赞
135
挺好
114
#软组织#
66
学习了
109
学习了
118
进来学习了
90
软组织肉瘤(Soft tissue sarcoms, STS)是指间叶起源的恶性病变。
80
#软组织肉瘤#近些年似乎不少了!这也是治疗的一个难题,#抗血管新生#治疗仍然是主要手段
173