BMJ:股骨颈骨折半髋置换术中严重骨水泥并发症发生率
2014-06-17 紫川秀第二 丁香园
对老年患者,股骨头骨折后行全髋置换已经成为一个相对成熟的术式。文献报道,过去一年发生在英国国内的因股骨头骨折而行半髋置换的患者已经接近23000例。关节置换术中使用骨水泥固定假体,提供良好的咬合力一直是关节置换中较为经典的方法。但是已经有较多文献报道骨水泥使用过程中会诱发较多并发症,如水泥或脂肪栓塞,过敏等,严重者可能使患者心脏停搏。【原文下载】 鉴于上述存在严重并发症可能性,有学者建议在置
对老年患者,股骨头骨折后行全髋置换已经成为一个相对成熟的术式。文献报道,过去一年发生在英国国内的因股骨头骨折而行半髋置换的患者已经接近23000例。关节置换术中使用骨水泥固定假体,提供良好的咬合力一直是关节置换中较为经典的方法。但是已经有较多文献报道骨水泥使用过程中会诱发较多并发症,如水泥或脂肪栓塞,过敏等,严重者可能使患者心脏停搏。【原文下载】
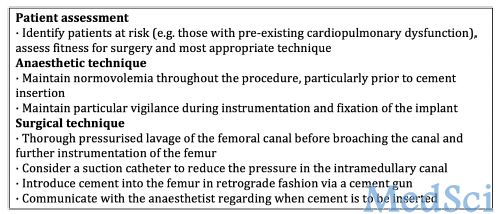
鉴于上述存在严重并发症可能性,有学者建议在置换过程中减少骨水泥的使用,英国国家患者安全机构2009针对术中使用骨水泥提供减少手术风险发生率的相关建议(图1),如术前详细评估患者病情,选择合适的手术技术;在麻醉时保证患者容量在正常水平,在灌注骨水泥时提高警觉;在扩髓或者填入骨水泥前对髓腔内容物进行盥洗,减小骨髓腔内的应力,注射骨水泥时速度适中等。
Paul教授收集了2005年-2012年英国NHS信息系统内有关患者安全不良反应的相关数据。所有明确报道和半髋关节置换术中骨水泥使用呈直接相关性的患者不良事件均纳入到本研究中。研究者设定结局指标为:主要指标为患者死亡(death),心脏骤停(arrest),接近心脏骤停(periarrest)等相关人数;次要指标包括:使用骨水泥后症状恶化的时间及相关功能预后。
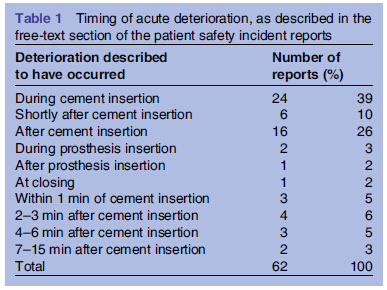
研究者共收集到62例报道和骨水泥使用直接相关的不良反应事件,约每2900例半髋置换术中发生一例,在62例严重不良事件中,41例患者直接死亡,14例患者心脏骤停后CPR成功,7例患者出现接近心脏骤停状态,大部分死亡事件(33/41)发生在手术台上。大部分病例(55/62)报道在使用骨水泥后即刻或很短时间内即发生恶化(表1)。随着时间推移,患者发生骨水泥严重并发症的数量在逐渐增加(图2),但这并不表示骨水泥相关的严重并发症发生率呈现上升趋势,因不同年份半髋关节置换术者的数量也不相同。
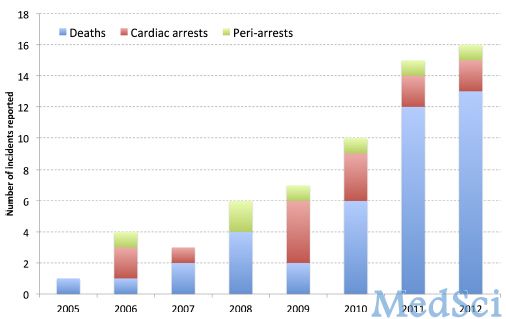
作者同时对英国国家患者安全机构颁布骨水泥注射注意事项前后时间段内相关严重并发症病例进行了对比研究,发现在注意事项发布后的患者死亡数量并不少于发布前患者的死亡数量,提示上述指南在临床实践中可能并没有得到很好的执行(表2)。

本研究的意义在于,明确股骨颈骨折术后半髋置换过程中骨水泥相关的严重并发症发生率,并重申英国国家患者安全机构骨水泥注意事项中有关麻醉医生和手术医生减少骨水泥相关并发症的相关措施的重要性。
原始出处:
Rutter PD1, Panesar SS2, Darzi A1, Donaldson LJ1.What is the risk of death or severe harm due to bone cement implantation syndrome among patients undergoing hip hemiarthroplasty for fractured neck of femur? A patient safety surveillance study.BMJ Open. 2014 Jun 12;4(6):e004853. doi: 10.1136/bmjopen-2014-004853.【原文下载】
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#发生率#
85
#BMJ#
95
#并发#
100
#置换#
88
#骨水泥#
84
#股骨颈#
70
#股骨#
77
#股骨颈骨折#
99
#置换术#
74