病例:这可不是肺结核,弄错了可就麻烦了!
2018-06-04 MedSci MedSci原创
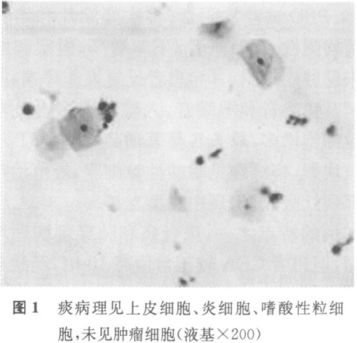
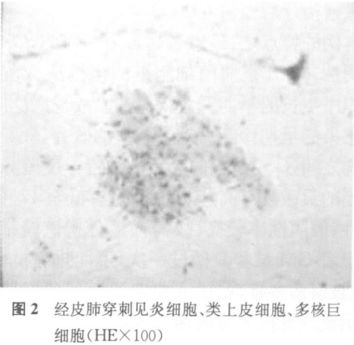
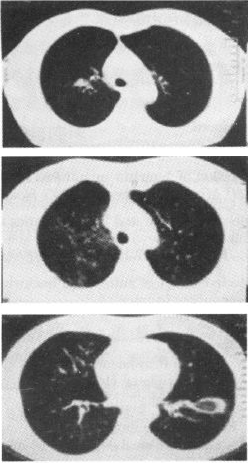
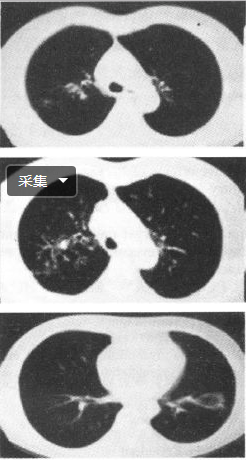
肺结核临床表现多样,故与其临床表现接近的肺部疾病有很多,但因肺结核比较常见,故很多较为罕见且类似肺结核的疾病容易被诊断为肺结核,误诊了的话治疗起来可就南辕北辙了!


本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











学习学习学习
75
#结核#
53
学习学习学习
73
厉害
78
学习了受益匪浅
88