Clinica Chimica Acta:用液滴数字PCR检测乳头状甲状腺癌细针穿刺液中BRAF V600E突变
2019-08-06 Gladiator MedSci原创
甲状腺乳头状癌<span lang="EN-US" style="font-size:12.0pt;mso-bidi-font-size:14.0pt;font-family:"Calibri","sans-serif"; mso-fareast-font-family:宋体;mso-bidi-font-family:"Times New Rom
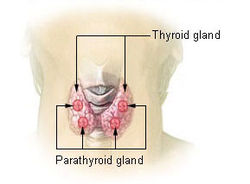
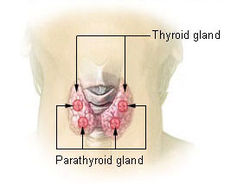
甲状腺乳头状癌(PTC) 是最常见的内分泌肿瘤,约占甲状腺癌的85%。对于PTC的诊断主要以超声引导下病理评价的细针穿刺(FNA)为标准检测手段,BRAF V600E突变是PTC发生、进展及临床病理特征较差的最常见分子标志物。然而,由于FNA获得的用于病理评价或BRAF V600E突变检测的肿瘤细胞数量较少,目前需要更灵敏、准确的方法。本研究旨在探讨液滴数字PCR (ddPCR)检测PTC患者FNA中BRAF V600E突变的效果。
本研究纳入160例疑似甲状腺癌患者,其中146例PTC患者,2例滤泡性甲状腺癌(FTC), 12例良性甲状腺肿瘤患者,根据NCCN甲状腺癌临床实践指南,经FNA活检确诊。采用ddPCR和扩增-难处理突变体系(ARMS,
AmoyDx)检测BRAFV600E突变,并对检测结果进行比较。
ddPCR高重现性(CV0.01% = 14.78%和CV10% = 4.85%)和检测灵敏度可以达到2-3拷贝/μl (0.06%)。在146例PTC患者中,检测到142例BRAF V600E突变,其中5例ARMS阴性,2例良性。
结果表明,ddPCR检测FNA液样BRAF V600E突变的灵敏度和准确性均高于ARMS法。
原始出处:
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#乳头状#
54
#CTA#
72
#乳头状甲状腺癌#
61
#V600E突变#
72
#穿刺#
79
#BRAF#
62
#PCR#
76
#PCR检测#
71