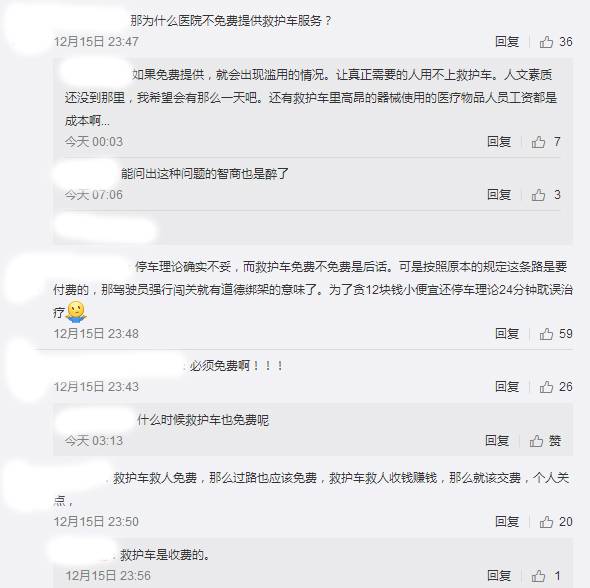
Lancet Respir Med:救护车上给予抗菌药物能延长脓毒症患者的生存期吗?
2017-12-26 应颖秋 环球医学
2017年发表于《Lancet Respir Med》的一项多中心、开放性、随机试验,考察了救护车中院前抗菌药物治疗对脓毒症患者的效果。
背景:紧急医疗服务(EMS)人员已经为改善对时间依赖性疾病患者的护理做出了重大贡献,如创伤和心肌梗死。脓毒症患者也可从及时的院前急救护理中获益。
方法:在培训EMS人员识别脓毒症后,研究者在服务荷兰34所二级和三级医院的10个大型区域救护车服务中进行了一项随机、对照、开放标签的试验。研究者对救护车早期抗菌药物给药与常规医疗进行了有效性的比较。使用大小为4的区组,用随机化方法按照1:1的比例将符合条件的患者随机分配至干预组(开放标签静脉头孢曲松2000mg+常规医疗)或常规医疗组(液体复苏+补氧),并根据区域对随机分组进行分层。首要结局为28天时的全因死亡率,并根据意愿治疗进行分析。为了评估培训的有效性,研究者确定了培训前和培训后,就诊中抗菌药物的平均使用时间(TTA)和EMS从业人员对脓毒症的认识。试验在ClinicalTrials.gov注册,编号NCT01988428。
结果:2698例患者于2014年6月30日~2016年6月26日入组。2672例患者纳入到意愿治疗分析中:干预组1535例,常规医疗组1137例。干预组在到达急诊前接受了中位26分钟(IQR,19~34)的抗菌药物。常规医疗组到达急诊后的中位TTA为70分钟(IQR,36~128),而EMS人员培训前(P=0.124),TTA为93分钟(IQR,39~140)。28天时,干预组和常规医疗组分别有120例(8%)和93例(8%)患者死亡(相对风险,0.95;95% CI,0.74~1.24)。干预组和常规组分别有102例(7%)和119例(10%)患者28天内再入院(P=0.0004)。发生了7例轻度过敏反应,无一例与头孢曲松相关。
结论:不同严重程度的脓毒症患者中,EMS从业人员培训可改善整个急性护理链中的早期认识和护理。然而,不管疾病的严重程度如何,在救护车上使用抗菌药物并不能提高生存率。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Lancet#
70
了解了解.学习学习
91
#抗菌#
69
#抗菌药#
73
#生存期#
72
#救护车#
85
#脓毒症患者#
68
#Med#
97
学习一下谢谢
92
学习一下谢谢
122