J Heart Lung Transplant:机械循环支持治疗女性患者预后较差
2016-10-30 MedSci MedSci原创
背景:机械循环支持(MCS)是一种广泛使用的管理策略。没有研究描述体外和持续MCS的性别差异。研究者应用入院数据分析体外和持续MCS住院预后的性别差异。方法:总的来说,使用国际分类疾病编码-9(临床修正)筛选出1994和2012之间进行MCS,有 1亿3450万的医院记录。主要不良事件(MAE)被定义为死亡、大出血、卒中、装置感染或机械并发症。根据INTERMACS的季度报告,在年度基础上确定IN
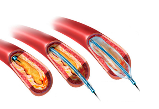
背景:机械循环支持(MCS)是一种广泛使用的管理策略。没有研究描述体外和持续MCS的性别差异。研究者应用入院数据分析体外和持续MCS住院预后的性别差异。
方法:总的来说,使用国际分类疾病编码-9(临床修正)筛选出1994和2012之间进行MCS,有 1亿3450万的医院记录。主要不良事件(MAE)被定义为死亡、大出血、卒中、装置感染或机械并发症。根据INTERMACS的季度报告,在年度基础上确定INTERMACS登记。使用多变量逻辑回归确定特征和预后之间的相关性。
结果:3523/4337例接受MCS设备患者有性别记录。这些患者来自45 INTERMACS网点和 (n = 1383)和246(n = 2954)非INTERMACS网点的患者,22%为女性。基线特征与女性年轻(33.5% vs 27.4%,年龄<50岁,P<0.001;平均55.7±17.3 vs 56.1±14.6岁)合并症较少显著相关。女性的住院死亡率(52.3% vs 40.8%,P<0.001)和MAEs(64.8% vs 52.5%,P<0.001)发生率更高。校正多变量的预测因素,女性发生MAEs的可能性为89%(P<0.001)。随着时间的推移,男性和女性的住院死亡率均下降,(相对风险减少10%/年,P<0.001),但在整个研究期间女性死亡率高于男性。
结论:接受MCS的患者,基本特征和预后有性别差异。女性患者有较高的住院死亡率及MAEs的风险升高,这不能以年龄或共发病来解释。需要进一步的研究这不相称的结果。
原始出处:
McIlvennan CK, Lindenfeld J, Kao DP. Sex differences and in-hospital outcomes in patients undergoing mechanical circulatory support implantation. J Heart Lung Transplant. 2016 Aug 20.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#女性患者#
90
#支持治疗#
114
#机械循环支持#
85
#plant#
68
#患者预后#
62
#TRA#
74
#Transplant#
73
介绍的很详细
89
#ART#
98
#HEART#
76