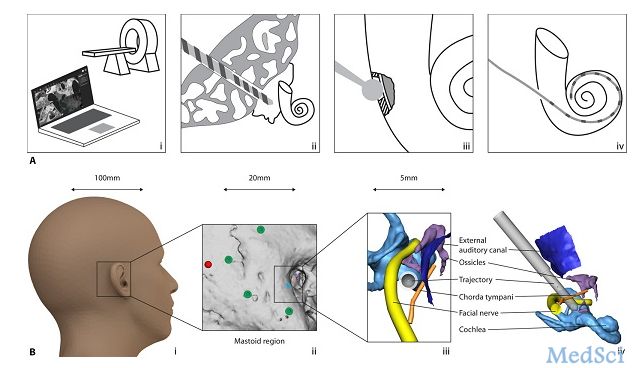
Sci Robot:全球首例!由机器人主刀的人工耳蜗植入手术顺利完成
2017-03-23 王晓行 动脉网
近日,《Science Robotics》网站发表一篇文章,伯尔尼大学的研发一款机器人,在它的辅助下,医生顺利完成了人工耳蜗植入手术,这次手术不同于以往的达芬奇那样的手术机器人:由医生操作手术臂进行手术,这款机器人是由医生监督,机器人“主刀”的手术。动脉网了解到,与人类相比,外科机器人系统在感知力、灵敏性以及手术规模上均优于人类,这些使得外科机器人天生就适合外科手术。另外,虽然科学界进行了深入的研


本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#植入手术#
73
#顺利完成#
79
#全球首例#
82
#人工耳蜗#
74
#机器人#
83
#植入#
76
#耳蜗植入#
67
#机器#
78