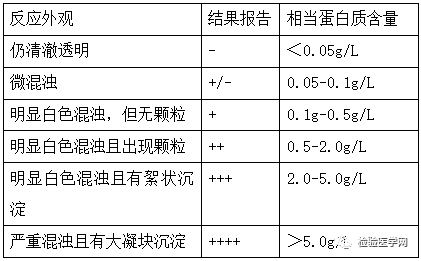
有些人小便时偶然间发现尿里面很多泡,有点像“啤酒花”,学医的容易跟食物过不去,如红细胞像武汉美食面窝,小儿腹泻呈蛋花汤样,还有酱油尿、巧克力囊肿、梨形心、葡萄胎、橘皮样变等,满满的画面感,即使餐桌上讨论学术问题也毫无违和感。 我们言归正传,这种“啤酒花”样的尿,泡泡比较多,气泡大小不一而且长时间不破裂,这时候就要去医院检查了。 那么是不是尿液里面起泡就是身体有问题呢?也可能是机械冲刷力起泡,尿速快,冲刷造成涡流,机械力也会产生泡沫,但这种泡沫数量少,留存时间短,若收集尿液快速搅动,可能一些泡沫加速破裂,这种泡沫很可能是机械力造成的。 需要警惕的几种情况 1.肝肾功能不全时,尿液混有较多量胆红素或蛋白质,表面张力增高,容易产生泡沫; 2.泌尿系感染或者膀胱肿瘤等使尿液成分复杂; 3.糖尿也可使尿液表面张力增高; 4.男性容易混有前列腺液、精液或者女性尿混有分泌物等也可造成表面张力增高。 在肾脏专科见的比较多的是蛋白尿,临床上早期无发热、尿频、尿急、尿痛,既往无糖尿病史,尿中异常泡沫反复出现,查蛋白尿阳性,预示肾脏出现了问题,这类情况往往起病比较隐匿。正常尿中蛋白量极少,张力低不容易起泡,但是在尿蛋白达到一定量时,尿就容易起泡,而且经久不散,这时就要去医院做24h尿蛋白定量,尿常规,肾功能等检查。那么就让我们来详细说说。 正常人肾小球滤液中具有一些小分子量蛋白,是通过肾小球滤膜的微小孔隙滤出,通过近端肾小管时绝大部分又重吸收,故终尿中蛋白质含量很少,一般为20-80mg/24h尿(随机1次尿液中含蛋白量仅为0-80mg/L),尿蛋白定性试验呈阴性,当某些因素引起尿蛋白含量大于150mg/24h尿,尿蛋白定性试验呈阳性,称为蛋白尿。 正常尿液中蛋白质按分子量可分为3种 1. 分子量大于90kD的蛋白质,含量极微,以肾小管上皮细胞分泌为主,占正常尿蛋白1/3,常见分泌型IgA和T-H糖蛋白; 2.分子量40-90kD的蛋白质,主要成分为白蛋白,所占比例为1/2-2/3; 3.分子量低于40kD的蛋白质,含量极少,常见α2微球蛋白、β2微球蛋白、免疫球蛋白Fc片段等,正常人滤液中大部分被重吸收。 尿蛋白对肾脏有危害,需规范治疗加以控制 1.尿蛋白的系膜毒性,引起肾小球硬化; 2.尿蛋白引起肾小管细胞生物学,改变其生长特性及其细胞因子的表达,诱导纤维化的过程; 3.尿蛋白引起小管间质缺氧严重,引起肾小管损伤。 为了疾病诊断和治疗,尿蛋白不同分类 1. 根据尿蛋白的量可分为肾病水平蛋白尿(≥3.5g/24h)和非肾病水平蛋白尿,为临床诊断提供依据; 2. 根据蛋白尿性质分为生理性蛋白尿和病理性蛋白尿,前者主要是一过性蛋白尿,肾脏无器质性病变,常小于0.5g/24h,后者多为持续性蛋白尿; 3. 根据蛋白尿中是否存在大量的大分子蛋白分为:选择性蛋白尿和非选择性蛋白尿,可以测定尿中IgG和转铁蛋白,IgG/转铁蛋白<0.1为选择性蛋白尿, 4. 根据蛋白尿形成机制分为: ·肾小球性蛋白尿,特点是尿蛋白排出量>2g/24h,成分以白蛋白等中大分子为主; ·肾小管性蛋白尿以小分子量蛋白(如β2微球蛋白)为主,一般蛋白定量<2g/24h,见于肾盂肾炎、抗菌药物、金属盐类、有机溶剂等引起的肾间质病变; ·混合型尿蛋白见于各种肾小球疾病后期,或全身性疾病同时侵犯肾小球和肾小管(如狼疮肾炎、糖尿病肾病、高血压肾病等); ·溢出性蛋白尿见于多发性骨髓瘤的轻链尿、横纹肌溶解的肌红蛋白尿、血管内溶血的血红蛋白尿等; ·组织性蛋白尿见于尿路炎症、肿瘤分泌蛋白,一般小于0.5g/24h; ·偶然性蛋白尿,见于肾脏本身无损害,而血液、脓液、或生殖系统分泌物混入尿液,导致尿蛋白定性试验阳性,规范操作或者短暂治疗后阴性,又称假性蛋白尿; ·直立性蛋白尿,将24h尿蛋白定量分为夜间8h卧位和白天16h立位,若24h尿蛋白定量>0.15g而8h卧位<0.05g,可以认定直立性尿蛋白。 检测尿蛋白的项目有 尿常规比较经济划算,随机尿就可以检测,推荐晨尿,可排除体位性蛋白尿,包含尿蛋白和尿微量白蛋白项目,有时容易粘液丝、前列腺液,阴道分泌物等干扰,所以建议复查。 干化学试纸法结果判读 试纸法测定不同标志性蛋白的低限 以磺基水杨酸法为例说明尿蛋白定性结果判读 24h尿蛋白定量是一个计算值,主要是收集24h尿测尿蛋白浓度乘以24h尿量,24h尿蛋白定量小于1g提示非肾小球疾病可能性大,常见肾盂肾炎、肾硬化、尿路梗阻、尿路肿瘤及结石等。尿蛋白介于1g-3g之间提示很可能是原发或者继发肾小球疾病,考虑是急性还是慢性,急性需要完善相关检查或者肾脏活检,进行积极治疗。尿蛋白大于3.5g是肾病综合征的诊断指标,也有可能是肾炎综合征,需要结合临床表现如有无水肿、白蛋白、血脂等综合分析。24h尿蛋白定量留取标本持续时间长,受患者依从性影响较大。 尿蛋白/肌酐比值也可检测随机尿,具有快速、简便、精确特点,为临床上理想的定性、定量诊断蛋白尿和随访的指标。1g尿蛋白/g尿肌酐,相当于尿蛋白1g/24h,预测24h尿蛋白量就方便得多。 特殊蛋白检查如尿蛋白电泳,可分辨出选择性蛋白尿和非选择性蛋白尿。多发性骨髓瘤的尿蛋白电泳检查对分型有帮助。 另外肾功能早期指标如胱抑素C,是一种半胱氨酸蛋白酶抑制剂,经肾小球滤过而被清除,是一种反映肾小球滤过率变化的内源性标志物,并在近曲小管重吸收,但重吸收后被完全代谢分解,不返回血液,较血清尿素、肌酐有更高的敏感性和特异性,还可以计算eGFR,一般人体表面积1.73m2计算,明确慢性肾脏疾病分期等。 有些特殊人群也会有蛋白尿,比如妊娠期女性,在妊娠早期尿蛋白阳性考虑非妊娠因素可能性大,但到晚期才出现阳性则可能是妊娠原因造成的,这种情况一般产后复查尿蛋白,若恢复阴性即可明确。 中草药如马兜铃等比较伤肾,如果在服用中药,建议定期检查肝肾功、尿蛋白等。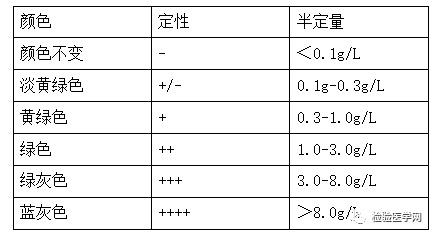
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








挺好的
105
#啤酒花#
61
精彩
132
👍🏻
133
好
118
学习了,谢谢分享!
148
分析得挺全面的
110