Stroke:警惕脑静脉血栓形成患者的毛刷征
2019-07-30 杨中华 脑血管病及重症文献导读
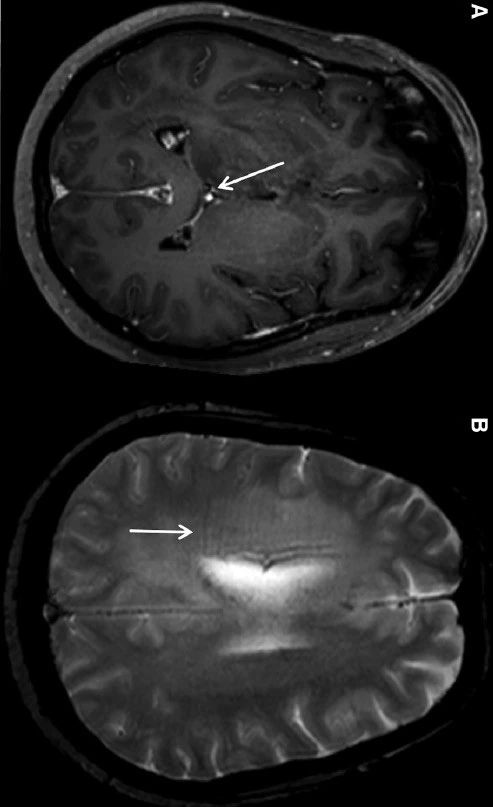
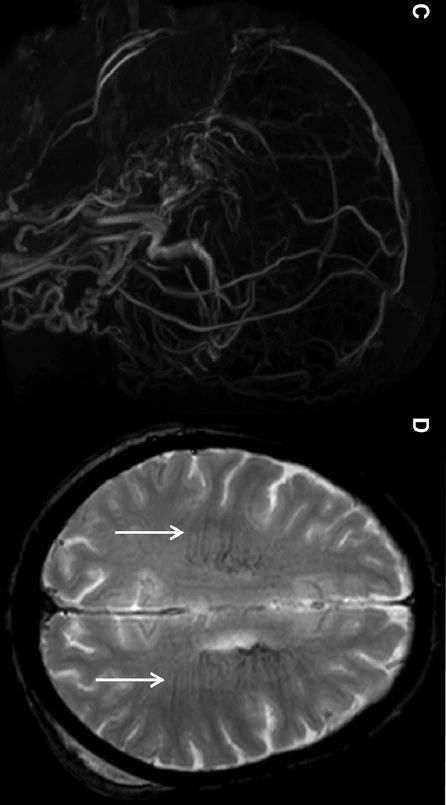
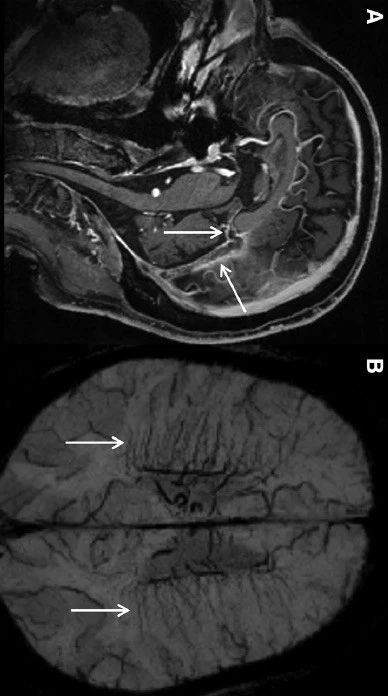
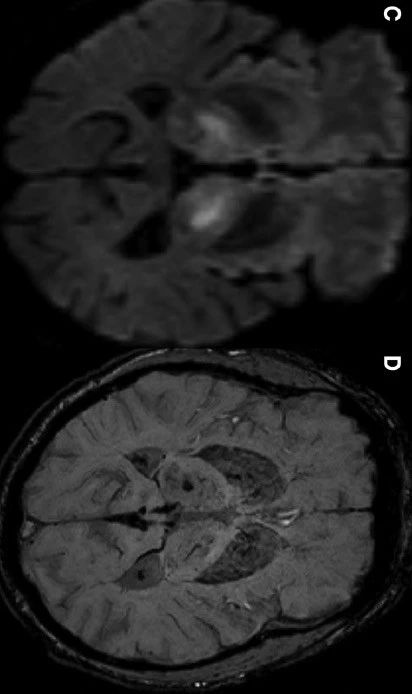
深部髓静脉位于侧脑室旁和侧脑室体部后部旁(located adjacent to the atrium and posterior body of the lateral ventricle),引流大脑半球白质的血液进入侧脑室的室管膜下静脉。他们是小静脉,在生理情况下,他们很难在常规 MRI 上显示。磁敏感 MR 序列(T2*和 SWI)能够较好地显示这些静脉,特别是静脉内脱氧血红蛋白水平升高时。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#静脉#
80
#静脉血#
73
#静脉血栓形成#
83
学习学习学习
95