偷拿21瓶医学中心研究样本回国!哈佛医学院中国访问学者被捕
2020-01-04 佚名 留美学子
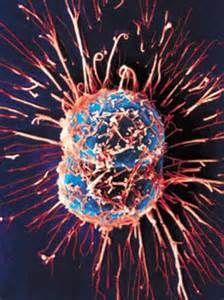
2019年12月30日波士顿联邦助理法官大卫亨尼斯(David Hennessy)裁定:郑灶松哈佛访问学者兼癌症研究员,试图非法走私、盗窃哈佛大学某医学中心实验室内的研究样本到中国。因担心其有潜逃风险,法官还批准被告不予保释。据《纽约时报》报道,郑灶松12月9日准备乘坐海南航空公司482次航班,由波士顿直飞北京,被美国海关在其托运行李中搜出21瓶咖啡色液体,瓶子都用玻璃纸包好藏在袜子当中,他12月
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#医学院#
54
#研究样本#
76
#样本#
72
#哈佛医学院#
92
#哈佛#
64