机器学习:准确率(Precision)、召回率(Recall)、F值(F-Measure)、ROC曲线、PR曲线
2019-07-14 不详 网络
在机器学习、数据挖掘、推荐系统完成建模之后,需要对模型的效果做评价。 业内目前常常采用的评价指标有准确率(Precision)、召回率(Recall)、F值(F-Measure)等,下图是不同机器学习算法的评价指标。下文讲对其中某些指标做简要介绍。 本文针对二元分类器! 本文针对二元分类器!! 本文针对二元分类器!!! 对分类的分类器的评价指标将在以后文章中介绍。 在介绍指标前
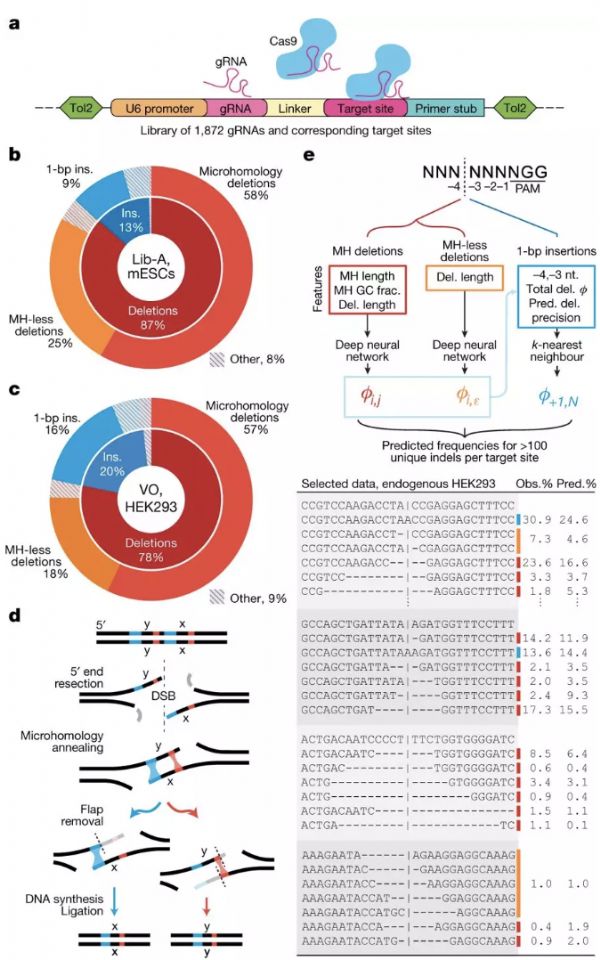
在机器学习、数据挖掘、推荐系统完成建模之后,需要对模型的效果做评价。 业内目前常常采用的评价指标有准确率(Precision)、召回率(Recall)、F值(F-Measure)等,下图是不同机器学习算法的评价指标。下文讲对其中某些指标做简要介绍。 本文针对二元分类器! 本文针对二元分类器!! 本文针对二元分类器!!! 对分类的分类器的评价指标将在以后文章中介绍。 在介绍指标前必须先了解“混淆矩阵”: 混淆矩阵 True Positive(真正,TP):将正类预测为正类数 True Negative(真负,TN):将负类预测为负类数 False Positive(假正,FP):将负类预测为正类数误报 (Type I error) False Negative(假负,FN):将正类预测为负类数→漏报 (Type II error) 1、准确率(Accuracy) 准确率(accuracy)计算公式为: 注:准确率是我们最常见的评价指标,而且很容易理解,就是被分对的样本数除以所有的样本数,通常来说,正确率越高,分类器越好。 准确率确实是一个很好很直观的评价指标,但是有时候准确率高并不能代表
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#ROC#
80
#ROC曲线#
90
#CIS#
0
#ALL#
89
#召回#
89
#机器#
65