JAMA:肿瘤坏死因子拮抗剂与癌症风险升高无关
2015-01-20 高晓方 翻译 中国医学论坛报
丹麦一项队列研究纳入56146例年龄≥15岁的炎症性肠病(IBD)患者,并对肿瘤坏死因子(TNF-α)拮抗剂暴露是否升高患者的癌症风险进行评估。结果显示,中位3.7年随访期间,TNF-α拮抗剂暴露和未暴露患者的癌症发病率分别为1.8%和6.7%。依据自首次TNF-α拮抗剂暴露时间和用药次数进行分析时,癌症风险均未出现显著升高。部位特异性癌症亦未显著增多。论文发表于《美国医学会杂志》。
丹麦一项队列研究纳入56146例年龄≥15岁的炎症性肠病(IBD)患者,并对肿瘤坏死因子(TNF-α)拮抗剂暴露是否升高患者的癌症风险进行评估。结果显示,中位3.7年随访期间,TNF-α拮抗剂暴露和未暴露患者的癌症发病率分别为1.8%和6.7%。依据自首次TNF-α拮抗剂暴露时间和用药次数进行分析时,癌症风险均未出现显著升高。部位特异性癌症亦未显著增多。论文发表于《美国医学会杂志》。
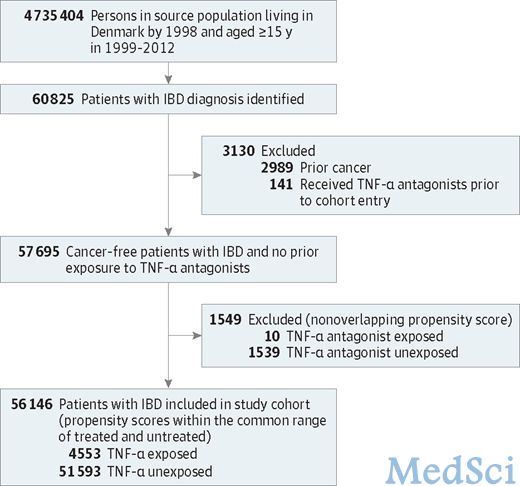
Figure 1.Formation of Study Cohort
点评:此结果与既往结论一致。尽管免疫抑制药物巯嘌呤可升高淋巴瘤和非黑色素瘤皮肤癌风险,但TNF-α拮抗剂与癌症风险升高无确定相关性。
原始出处:本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#坏死#
58
#肿瘤坏死因子#
76
#拮抗剂#
63