JAHA:间歇性禁食可增强肺动脉高压个体右心室功能
2021-11-09 MedSci原创 MedSci原创
IF直接增强了PAH动物的RV功能并重组了肠道微生物组。这些结果表明IF可能是对抗RV功能障碍的一种非药物治疗手段。
间歇性禁食(IF)具有多效性心血管益处,包括重组肠道微生物组分和增强细胞代谢。肺动脉高压(PAH)是一种罕见的致命性疾病,其特征是右心室(RV)线粒体功能障碍以及由此产生的脂毒性和微生物群失调。然而,IF对PAH患者RV功能的影响尚未明确。

近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员分析了IF如何改变经野百合碱诱导的PAH模型的肠道微生物群组成、RV功能和存活率情况。

雄性SpragueDawley大鼠被随机分为3组:对照组、野百合碱喂养组和野百合碱喂养+IF(隔日喂养)。
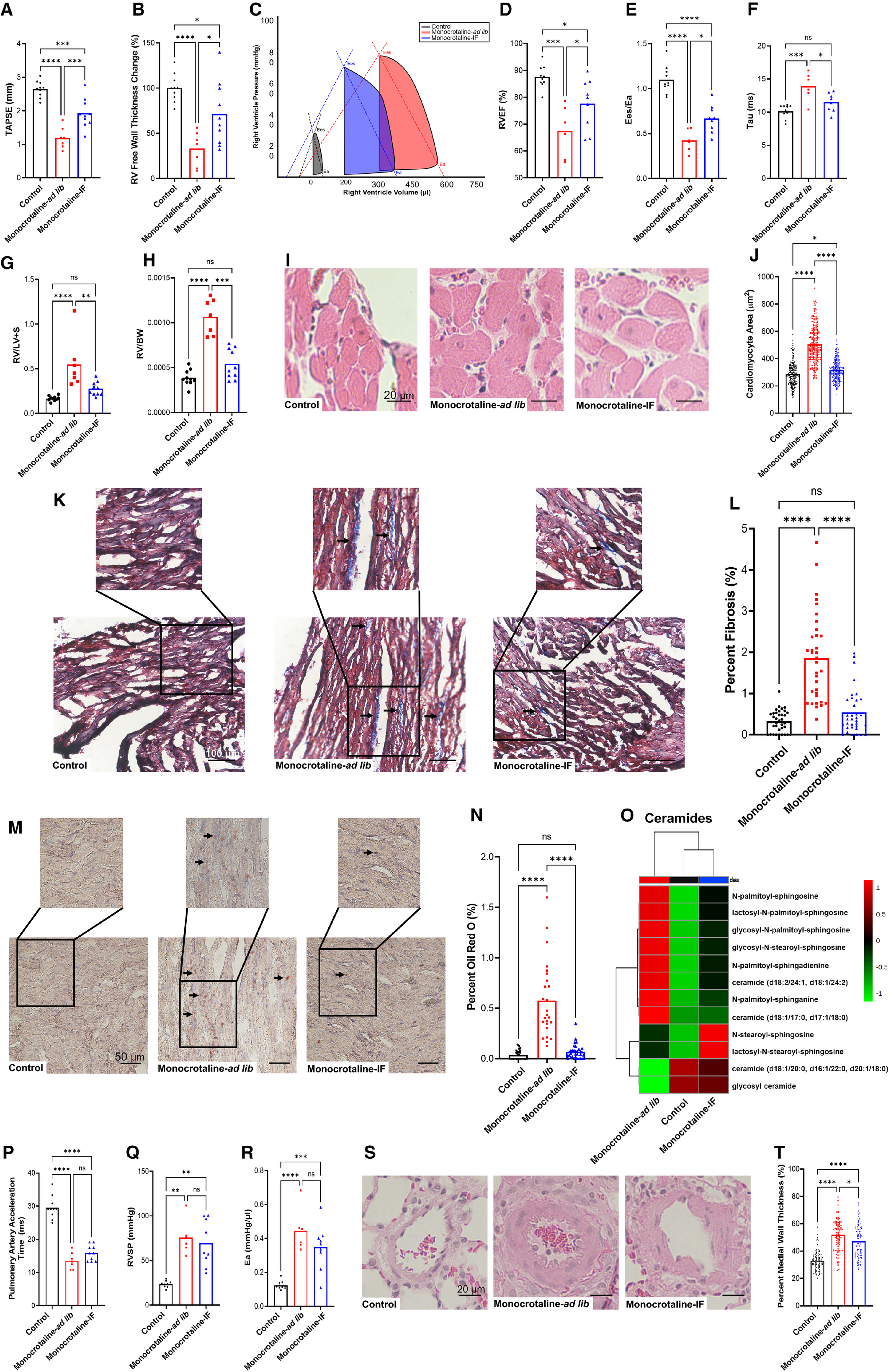
研究部人员通过超声心动图和有创血流动力学发现IF改善了RV收缩和舒张功能,尽管PAH的严重程度没有显著变化。IF可防止过早死亡(野百合碱喂养诱导的PAH组死亡率为30%,而野百合碱喂养+IF组大鼠的死亡率为0%,P=0.04)。IF降低了RV心肌细胞肥大并减少了RV纤维化。IF阻止了经油红O染色的RV脂质积累和代谢组学确定的神经酰胺积累。与野百合碱喂养组相比,IF减轻了空肠绒毛长度和杯状细胞丰度。16S核糖体RNA基因测序证明IF改变了肠道微生物组。特别是,野百合碱+IF大鼠中乳酸杆菌的丰度增加。代谢组学分析显示,IF降低了RV微生物组代谢物的水平,包括胆汁酸、芳香族氨基酸代谢物和γ-谷氨酸化氨基酸。
由此可见,IF直接增强了PAH动物的RV功能并重组了肠道微生物组。这些结果表明IF可能是对抗RV功能障碍的一种非药物治疗手段。
原始出处:
Sasha Z. Prisco.et al.Intermittent Fasting Enhances Right Ventricular Function in Preclinical Pulmonary Arterial Hypertension.JAHA.2021.https://www.ahajournals.org/doi/10.1161/JAHA.121.022722
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#动脉高压#
40
#右心室功能#
47
#间歇性#
48
#AHA#
40
#右心室#
56
谢谢分享
99
好好
0