有症状的股骨髋臼撞击关节镜矫正后 10 年的存活率和临床结果
2022-01-18 MedSci原创 MedSci原创
股骨髋臼撞击 (FAI) 是一种常见的机械性髋关节疾病,在运动员和普通人群中都很普遍。手术干预是一种有效的治疗选择,可在中短期随访中改善症状和功能。而文献中很少有研究报告关节镜手术的长期成功结果。
股骨髋臼撞击 (FAI) 是一种常见的机械性髋关节疾病,在运动员和普通人群中都很普遍。手术干预是一种有效的治疗选择,可在中短期随访中改善症状和功能。而文献中很少有研究报告关节镜手术的长期成功结果。
该研究的目的是量化接受关节镜治疗的症状性 FAI 患者的 10 年生存率和临床结果。

图1 文章来源
该研究团队所登记髋关节患者 (n = 119) 完成了患者报告的结果测量 (PROM),包括修改后的 Harris 髋关节评分 (mHHS)、加州大学洛杉矶分校 (UCLA) 活动量表、36 项简短健康调查 (SF- 36),西安大略和麦克马斯特大学骨关节炎指数(WOMAC)在关节镜检查后至少 10 年(范围,10-12 年),并使用 Wilcoxon 符号秩检验将结果与基线分数比较。
使用卡方分析分析了几个预后因素之间的关联,包括年龄、性别、Tönnis 分级和盂唇
治疗,以及随后转换为全髋关节置换术 (THR) 或重复髋关节镜检查 (RHA)。还使用 Pearson 相关分析检查了运动范围和放射学结果与临床结果之间的关系。
使用分布法(变化评分的 0.5 标准差)计算最小临床重要差异 (MCID),使用锚定法确定显着临床获益 (SCB)。最后,使用接受者操作特征曲线和随后的约登指数来确定 PROM 的截止值,这相当于患者可接受的症状状态 (PASS)。
结果显示,共有 8.4% 的病例需要转换为 THR,5.9% 的病例需要 RHA。术后 10 年观察到 mHHS、SF-36 和 WOMAC 评分显着改善,满意度高(90%)。
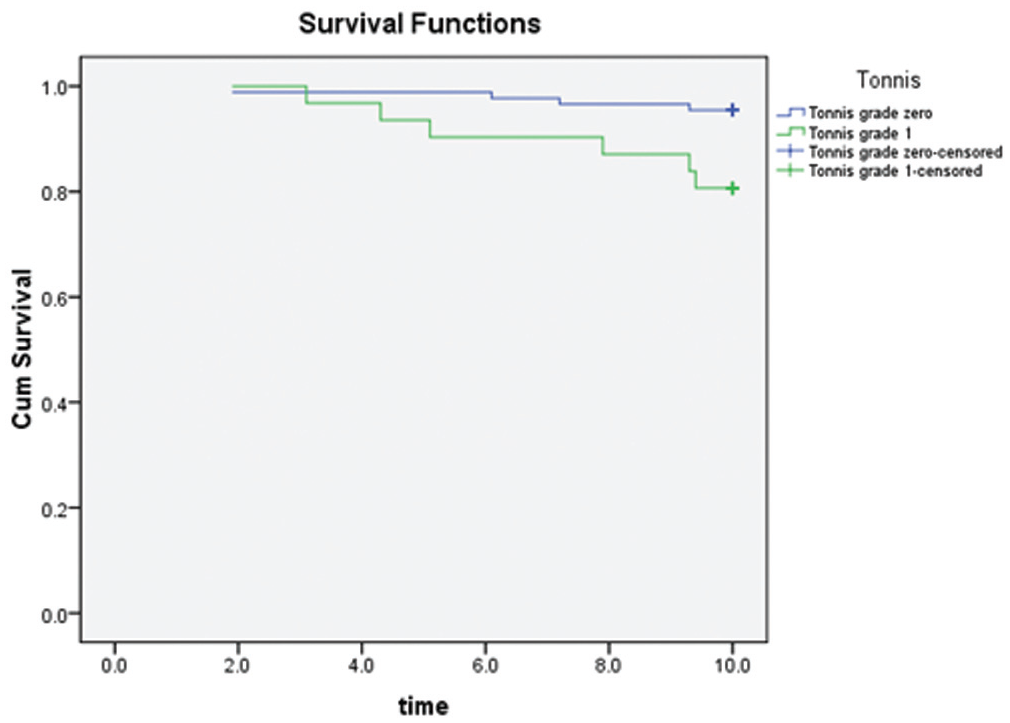
图 2Kaplan-Meier 曲线表示基于 Tönnis 等级的随时间(年)的累积 (Cum) 存活率
尽管患者术后已过10 年,但活动水平(UCLA 评分)没有显着变化。高比例的患者在 mHHS (88%)、SF-36 (84%) 和 WOMAC (60%) 方面实现了 MCID。大多数患者还达到了 PASS(mHHS 为 62%,UCLA 为 85%,SF-36 为 78%,WOMAC 为 84%)和 SCB(mHHS 为 74%,UCLA 为 58%,SF-36 为 52% ,而 WOMAC 为 56%)。
对于有症状的 FAI 患者,关节镜干预是一种安全可行的治疗选择,患者可以期待长期改善和高满意度。结果表明,在初次手术后 10 年,患者的满意度(90%)和存活率(91.6%)很高,临床结果非常好。
原始文章:
Carton P, Filan D, Mullins K. Survivorship Rate and Clinical Outcomes 10 Years After Arthroscopic Correction of Symptomatic Femoroacetabular Impingement. Am J Sports Med. 2022 Jan;50(1):19-29. doi: 10.1177/03635465211055485. Epub 2021 Nov 19. PMID: 34796726.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#临床结果#
97
#存活率#
80
#关节镜#
113
#股骨#
118