J CLIN ONCOL:初诊急性髓系白血病伊达比星和大剂量柔红霉素诱导化疗方案比较的前瞻性研究
2017-06-21 xuyihan MedSci原创
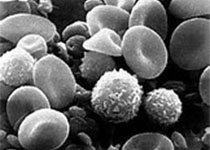
最近有研究比较了伊达比星(12mg/m2/d,3天)与大剂量柔红霉素(90mg/m2/d,3天)这两种诱导方案在初诊急性髓系白血病(AML)的年轻患者中的疗效。
最近有研究比较了伊达比星(12mg/m2/d,3天)与大剂量柔红霉素(90mg/m2/d,3天)这两种诱导方案在初诊急性髓系白血病(AML)的年轻患者中的疗效。
本项试验分析了共299例患者(149例随机分为阿糖胞苷加伊达比星[AI],150例分为大剂量柔红霉素加阿糖胞苷[AD])。所有患者接受阿糖胞苷(200 mg/m2/d ,7天)。
研究结果显示:232例(77.6%)发生了完全缓解(CR),在AI与AD组之间CR率并没有差异(分别为80.5% V 74.7%,P = .224)。在34.9个月的中位随访时间、生存率和复发率在AI和AD组之间没有不同(4年生存率,51.1% V 54.7%;P = .756;累积复发率,35.2% V 25.1%;P =. 194;无事件生存率,45.5% V 50.8%;P=.772)。两组的毒性反应也相似。有意思的是,有FLT3内部串联重复(ITD)突变的患者的总体生存期和无事件生存期大有不同(AI V AD:中位总体生存期,分别为15.5个月 V 15.5个月不到;P=.030;无进展生存期,分别为11.9个月 V 11.9个月不到;P=.028)。
此项比较伊达比星和大剂量柔红霉素诱导方案的III期试验,发现两者之间的CR率、复发和生存期并没有显着差异。治疗组与FLT3-ITD突变之间存在交互作用,有FLT3-ITD突变的患者大剂量柔红霉素较伊达比星更有效。
原始出处:
Je-Hwan Lee.et al.Prospective Randomized Comparison of Idarubicin and High-Dose Daunorubicin in Induction Chemotherapy for Newly Diagnosed Acute Myeloid Leukemia.J CLIN ONCOL.2017
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#Oncol#
119
#红霉素#
113
#前瞻性研究#
106
#髓系白血病#
93
#前瞻性#
100
#诱导化疗#
111
#大剂量#
84
不错不错
126