2019年遗传代谢紊乱学会年会:Pegzilarginase治疗精氨酸酶基因缺失患者的阳性I/II期临床数据
2019-04-08 不详 网络
Aeglea是一家临床阶段的生物技术公司,致力于为罕见的遗传性疾病和癌症患者设计和开发创新的酶疗法,近日宣布将在2019年遗传性代谢紊乱学会(SIMD)年会上公布pegzilarginase治疗精氨酸酶基因缺失的最新I/II期临床的阳性数据。
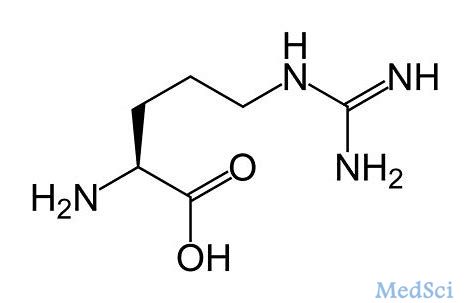
Aeglea是一家临床阶段的生物技术公司,致力于为罕见的遗传性疾病和癌症患者设计和开发创新的酶疗法,近日宣布将在2019年遗传性代谢紊乱学会(SIMD)年会上公布pegzilarginase治疗精氨酸酶基因缺失的最新I/II期临床的阳性数据。精氨酸酶是催化水解L-精氨酸生成鸟氨酸与尿素的反应酶,如果精氨酸酶基因缺失,患者血浆中精氨酸浓度将异常升高。
I/II期临床证明了pegzilarginase可持续降低血浆精氨酸浓度,且患者对治疗通常耐受良好。超敏反应很少发生,即使发生也可通过标准手段进行控制,因此不会导致治疗中止。
原始出处:
http://www.firstwordpharma.com/node/1633819?tsid=4#axzz5kSaSXmAK
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#临床数据#
27
#精氨酸#
45
#基因缺失#
51
#PE#
32
#I期临床#
25
#GINA#
35
#II期临床#
23
#PEG#
0