Sci Rep:世界阿尔茨海默病日:口服药物,或破阿尔茨海默症治疗僵局
2019-09-21 顾露露 生物探索
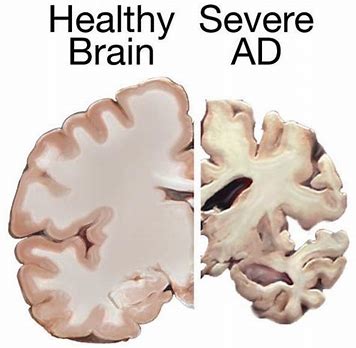
阿尔茨海默症(Alzheimer‘s disease)导致神经细胞死亡,随着时间推移,大脑急剧萎缩,细胞破坏导致记忆力衰退、性格改变以及日常活动的问题。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#阿尔茨海#
68
#阿尔茨#
68
#口服药#
77
#口服药物#
86
#阿尔茨海默#
69
向科研人员致敬
117