Nature:华人团队发现最凶险乳腺癌的“帮凶”,打掉它就能攻入肿瘤内部
2021-11-05 “ 生物世界”公众号 “ 生物世界”公众号
乳腺癌,是女性中最常见的癌症,而在2020年,乳腺癌取代肺癌,已成为全球第一大癌症,WHO国际癌症研究署(IARC)发布的2020年全球最新癌症负担数据显示,2020年全球乳腺癌新发病例高达226万例
乳腺癌,是女性中最常见的癌症,而在2020年,乳腺癌取代肺癌,已成为全球第一大癌症,WHO国际癌症研究署(IARC)发布的2020年全球最新癌症负担数据显示,2020年全球乳腺癌新发病例高达226万例,死亡68万例。在我国,乳腺癌的发病率也在逐年提升,据WHO预测,2020年中国新增乳腺癌病例高达41万。
乳腺癌大多预后良好,但是大约10%-20%的乳腺癌为三阴性乳腺癌,这类乳腺癌由于雌激素受体(ER)、孕激素受体(PR)、人表皮生长因子受体-2(HER-2)缺乏而得名,三阴性乳腺癌是最具侵袭性和致命性的乳腺癌,更容易扩散转移,易复发,而且由于缺少治疗靶点,治疗药物有限,一直是乳腺癌治疗的难点。
2021年11月3日,乔治·华盛顿大学 Li Rong、得克萨斯大学安志强等人在 Nature 发表了题为:Tumour DDR1 promotes collagen fibre alignment to instigate immune exclusion 的研究论文。
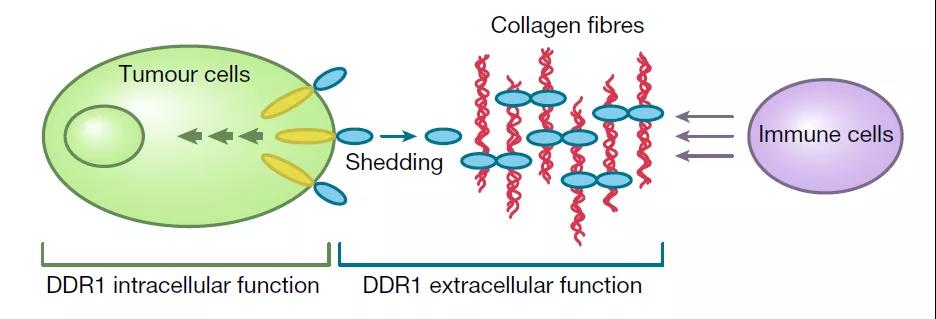
该研究发现,在人类三阴性乳腺癌中,DDR1基因的表达与肿瘤内抗肿瘤T细胞的丰度呈负相关,进一步揭示了DDR1基因可以防止免疫细胞进入肿瘤内部杀伤癌细胞。而敲除DDR1基因或通过抗体抑制DDR1,就能打破三阴性乳腺癌的防线,让免疫细胞成功穿越,清除肿瘤细胞。这一发现为三阴性乳腺癌的能够侵袭性乳腺癌的新疗法铺平了道路。
研究团队发现,在人类三阴性乳腺癌中,DDR1基因的表达与肿瘤内抗肿瘤T细胞的丰度呈负相关。在癌症发展过程中,DDR1就像是围绕在肿瘤外部的带刺铁丝网,阻挡了免疫细胞攻入肿瘤内部。

三阴性乳腺癌,约占所有乳腺癌的10%-20%,这类乳腺癌由于缺乏癌症治疗中的常用靶向受体,导致难以使用靶向药治疗。近年来发展起来的肿瘤免疫疗法,旨在激活免疫细胞来杀伤肿瘤,但是DDR1就像一道屏障阻止了免疫细胞进入肿瘤内部发挥杀伤作用。
研究团队在多个临床前动物模型中评估了敲除DDR1基因的影响,实验结果表明,敲除DDR1基因不仅可以阻止肿瘤生长,还可以保护身体免受未来肿瘤的侵害。
鉴于这些新发现,共同通讯作者安志强团队开发了一种治疗性的DDR1靶向抗体,靶向抑制DDR1,可以打破肿瘤防线,帮助免疫细胞成功穿越到肿瘤内部,进而消灭肿瘤细胞。

研究团队表示,这项研究发现并证实了DDR1在癌症中的重要作用,很可能为三阴性乳腺癌带来新的治疗途径,这项研究可以说是基础研究和转化研究协同的典范,从基础研究发现到快速开发候选药物,将为众多侵袭性乳腺癌患者带来希望。
通讯作者Li Rong教授
原始出处:
Sun, X., Wu, B., Chiang, HC. et al. Tumour DDR1 promotes collagen fibre alignment to instigate immune exclusion. Nature (2021). https://doi.org/10.1038/s41586-021-04057-2.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#Nat#
144
期待
218
#华人#
109
谢谢分享
206