Nat Genet:大规模研究发现可能增加卵巢癌风险的新变异
2017-03-29 生物谷 生物谷
近日一项研究通过对大约10万人DNA测序结果进行分析,其中包括17000名卵巢癌病人,发现12个新的基因变异可能增加一种常见卵巢癌的患病风险并证实了18个之前曾经报道过的基因变异与这种卵巢癌的发生存在关联。相关研究结果发表在国际学术期刊Nature Genetics上。来自剑桥大学的Paul Pharoah教授解释道:“我们知道对女性来说,
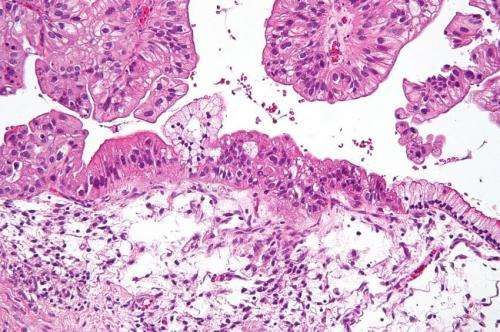
近日一项研究通过对大约10万人DNA测序结果进行分析,其中包括17000名卵巢癌病人,发现12个新的基因变异可能增加一种常见卵巢癌的患病风险并证实了18个之前曾经报道过的基因变异与这种卵巢癌的发生存在关联。
相关研究结果发表在国际学术期刊Nature Genetics上。
来自剑桥大学的Paul Pharoah教授解释道:“我们知道对女性来说,遗传因素占卵巢癌患病风险的大约三分之一。我们还不太确定增加患癌风险的环境因素到底包括哪些,但是我们知道有些因素可以降低卵巢癌患病风险,包括服用口服避孕药,输卵管结扎以及生育。”
类似BRCA1和BRCA2这样发生遗传错误的基因占遗传因素的大约40%。这些基因错误在人群中比较罕见(大约每300人中有1人携带)并且与卵巢癌以及卵巢癌的高发风险相关。而一些常见的基因变异被认为占剩余遗传因素的主要部分。
在OncoArray Consortium项目之前,研究人员已经在基因组中发现了27个与卵巢癌风险相关的常见变异,但是其中一些只与一些罕见的卵巢癌亚型相关。OncoArray Consortium项目研究了超过25000名上皮卵巢癌病人,并对大约41000名健康对照进行了比较。他们随后又分析了31000名BRCA1和BRCA2突变携带者,其中包括大约4000名上皮卵巢癌病人。经过分析研究人员发现了12个与上皮卵巢癌发生风险相关的新变异,并且证实了18个之前曾经报道过的变异。
到现在为止一共有30个已知的风险变异,这些基因变异占遗传因素的6.5%。“卵巢癌是一种复杂疾病,即使我们现在已经知道了30个增加患病风险的基因变异,但仍然只占遗传因素的一小部分。我们相信还有更多基因变异参与其中,其中大部分都是常见变异,还有一些是罕见变异。”来自美国墨菲特癌症中心的Dr. Catherine Phelan这样说道。
研究人员指出虽然通常认为我们的基因会影响疾病风险,而事实上大多数基因变异都没有落在负责蛋白编码的基因内部,而是落在人类基因组的非编码区域,这些区域并不会编码蛋白,而主要负责调解基因的活性。
由于这些基因变异比较常见,一些女性可能会同时携带多个风险基因变异。但是即使这些变异联合在一起也不会对患病风险产生很大影响,研究人员这样解释道。即使是携带变异数目最多的女性其卵巢癌终生风险也只有2.8%。
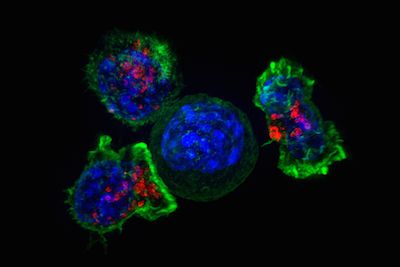
“我们现在对于这些基因变异究竟会在分子和细胞水平上产生什么样的功能影响仍然一无所知,对于它们如何影响患癌风险也仍然不了解。如果我们可以理解这些变异如何发挥作用,将有望找到更好的卵巢癌预防和治疗策略。”来自美国希德斯西奈医疗中心的Dr . Simon Gayther这样表示。
原始出处:
Catherine M Phelan et al, Identification of 12 new susceptibility loci for different histotypes of epithelial ovarian cancer, Nature Genetics (2017). DOI: 10.1038/ng.3826
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#新变异#
58
#癌风险#
93
#Genet#
89
#大规模#
87
#Nat#
100
#Gene#
70
#研究发现#
81
#变异#
75
如果我们可以理解这些变异如何发挥作用,将有望找到更好的卵巢癌预防和治疗策略。
116
文章很好,值得分享
115