JCC: 低白蛋白血症与接受回结肠切除术的克罗恩病患者的术后并发症发生有关
2021-07-14 MedSci原创 MedSci原创
虽然目前生物制剂的广泛使用使得克罗恩病患者的治疗效果有了很大的进步,但是克罗恩病患者的手术率并没有得到很好的降低。回盲部切除术吻合术仍然是 CD 最常见的手术。
虽然目前生物制剂的广泛使用使得克罗恩病患者的治疗效果有了很大的进步,但是克罗恩病患者的手术率并没有得到很好的降低。回盲部切除术吻合术仍然是 CD 最常见的腹腔内手术。由于免疫治疗对手术结果的潜在影响,早期回顾性研究认为术前生物暴露对围手术期或术后并发症(腹内脓毒症并发症 [IASC] 和浅表手术部位感染)具有负面影响。因此,本项研究旨在对此进行深入研究。

研究人员收集了2009 年至 2019 年期间接受回结肠切除术的克罗恩病患者的临床资料。手术前后 12 周内未使用生物制剂被归类为无生物制剂组,而使用过抗肿瘤坏死因子、维多珠单抗或优特克单抗的患者被归为生物制剂暴露组。主要观察终点是 90 天腹内脓毒症并发症。危险因素包括术前药物治疗、人口统计学、疾病特征、实验室检查结果和手术方法。回归模型评估了生物制剂使用与腹腔内脓毒症并发症的关联。

本项研究共纳入了 815 名接受回结肠切除术的克罗恩病患者 [62% 无生物制剂,31.4% 抗肿瘤坏死因子,3.9% 维多珠单抗,2.6% 优特克单抗]。85.9% 的患者主要以缝合 [77.2%] 的方式进行了初次肠吻合。41.4% 的患者使用了微创方法。810例患者术后90天腹腔内脓毒症率为12%,脓肿率为9.6%,吻合口漏率为3.2%。多变量回归建模控制混杂变量表明,具有抗肿瘤坏死因子的生物术前使用[p= 0.21],维多珠单抗[ p= 0.17],或优特克单抗[p= 0.52] 与腹腔内脓毒症并发症没有显着相关性。术前白蛋白 < 3.5 g/dl 与腹腔内脓毒症并发症独立相关(比值比 [OR] 1.76 [1.03, 3.01])。
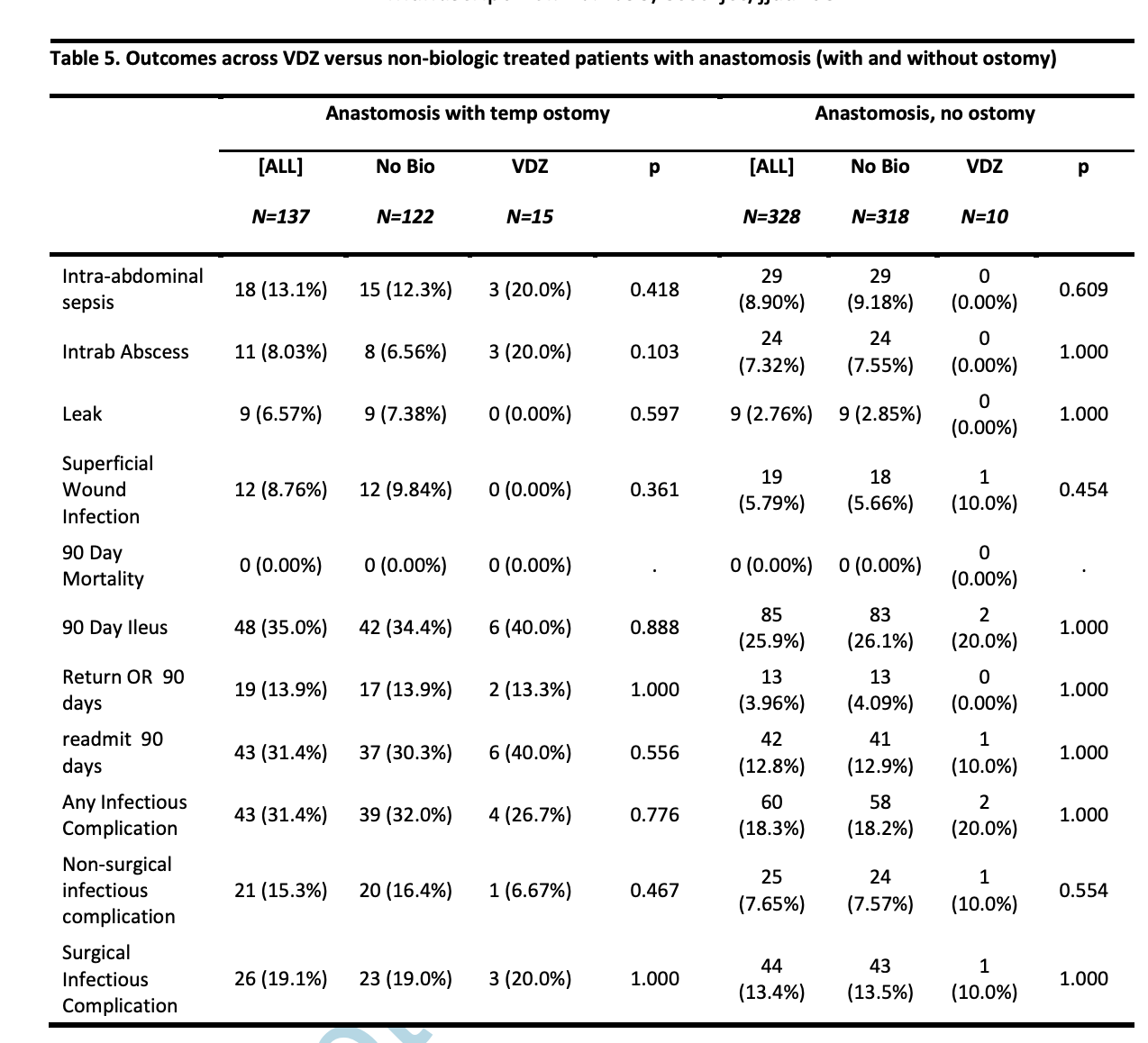
图:影响术后并发症的多因素回归分析
本项研究证实在接受回结肠切除术的克罗恩病患者中,术前生物制剂与术后 90 天腹腔内脓毒症并发症无关。术前生物暴露不应延误必要的手术。
原始出处:
Ravi S Shah. Et al. Hypoalbuminaemia, Not Biologic Exposure, Is Associated with Postoperative Complications in Crohn’s Disease Patients Undergoing Ileocolic Resection. Journal of Crohn's and Colitis.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#切除术#
65
#结肠切除术#
92
#并发#
70
#白蛋白#
93
学习
141