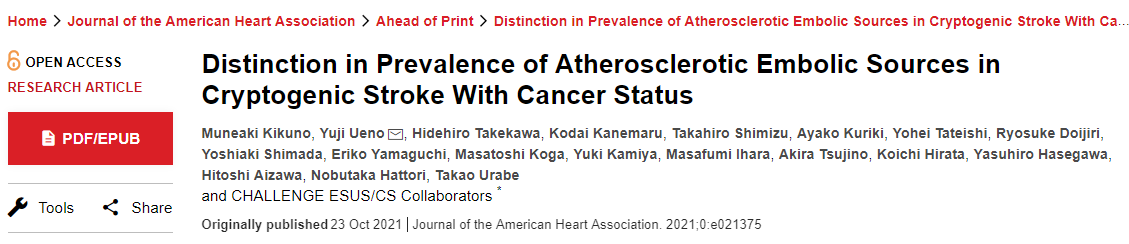
JAHA:隐源性卒中患者动脉粥样硬化栓塞患病率的区别
2021-10-24 MedSci原创 MedSci原创
癌症患者在隐源性卒中中并不少见。虽然活动性癌症患者有更多的多发性梗死,但非活动性癌症患者伴有更多的动脉粥样硬化栓塞来源,可能导致动脉性卒中。
脑血管疾病是癌症患者常见的合并症。尽管活动性癌症通过多种病理状况导致缺血性卒中,包括可归因于Trousseau综合征的血栓栓塞,但卒中与非活动性癌症之间的关系知之甚少。
近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,该研究的目的是阐明活动性和非活动性癌症患者隐源性卒中的不同潜在发病机制,并通过经食道超声心动图进行详细调查。
经食道超声心动图对不明来源栓塞性卒中/隐源性卒中的栓塞性卒中机制(CHALLENGE ESUS/CS)登记研究是一个多中心注册,包括最初诊断为隐源性卒中并接受经食管超声心动图检查的患者的数据。研究人员将患者分为活动性癌症、非活动性癌症和非癌症组,并比较它们的临床特征。
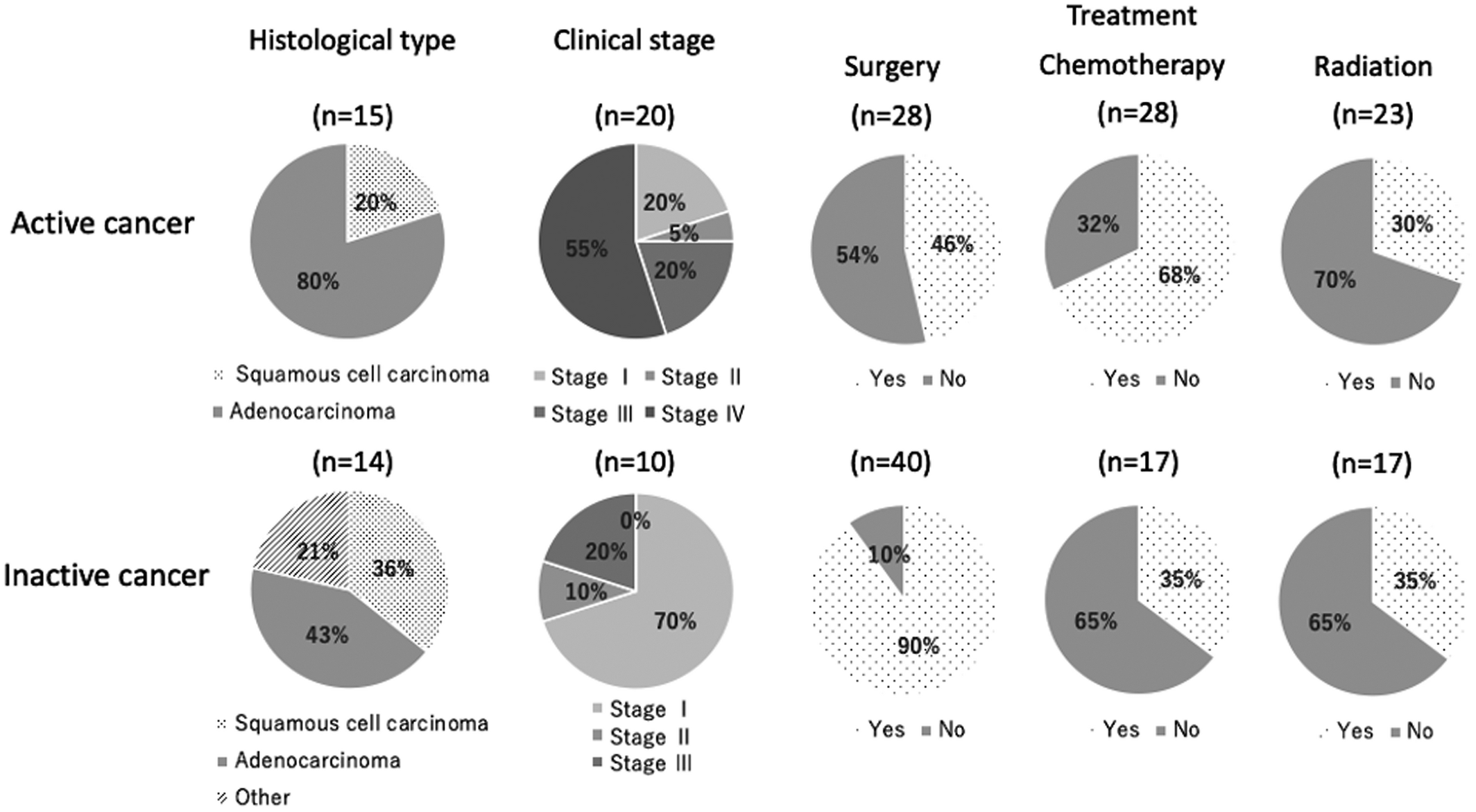
该研究总共纳入了667名登记患者(年龄为68.7±12.8岁;455名男性),41名(6.1%)患有活动性癌症,51名(7.5%)有非活动性癌症病史。在多项Logistic回归分析中,多个血管区域的梗死(比值比[OR]为2.73;95%CI为1.39-5.40)和CRP(C反应蛋白)(OR为1.10;95%CI为1.01-1.19)与活动性癌症独立相关,而年龄(OR为1.05;95%CI为1.01-1.08)、中风病变导致对侧颈动脉狭窄(OR为4.05;95%CI为1.60-10.27)、主动脉瓣钙化(OR为2.10;95%CI为1.09-4.05)和主动脉弓复杂病变(OR为2.13;95%CI为1.11-4.10)与非活动性癌症显著相关。
由此可见,癌症患者在隐源性卒中中并不少见。虽然活动性癌症患者有更多的多发性梗死,但非活动性癌症患者伴有更多的动脉粥样硬化栓塞来源,可能导致动脉性卒中。
原始出处:
Muneaki Kikuno.et al.Distinction in Prevalence of Atherosclerotic Embolic Sources in Cryptogenic Stroke With Cancer Status.JAHA.2021.https://www.ahajournals.org/doi/10.1161/JAHA.120.021375
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#隐源性卒中#
72
#粥样硬化#
79
#卒中患者#
80
#患病率#
87
#AHA#
119
学习了
108
??
107